Subdural Hematoma
Background
A subdural hematoma (SDH) is a collection of blood below the inner layer of the dura but external to the brain and arachnoid membrane. Subdural hematoma is the most common type of traumatic intracranial mass lesion.
Subdural hematoma occurs not only in patients with severe head injury but also in patients with less severe head injuries, particularly those who are elderly or who are receiving anticoagulants. Subdural hematoma may also be spontaneous or caused by a procedure, such as a lumbar puncture. Rates of mortality and morbidity can be high, even with the best medical and neurosurgical care.
Subdural hematomas are usually characterized by their size and location and the amount of time elapsed since the inciting event age (i.e., whether they are acute, subacute, or chronic). When the inciting event is unknown, the appearance of the hematoma on neuroimaging studies can help determine when the hematoma occurred. These factors, as well as the neurologic and medical condition of the patient, determine the course of treatment and may also influence the outcome.
Generally, acute subdural hematomas are less than 72 hours old and are hyperdense compared with the brain on CT scans. The subacute phase begins 3-7 days after acute injury. Chronic subdural hematomas develop over the course of weeks and are hypodense compared with the brain. However, subdural hematomas may be mixed in nature, such as when acute bleeding has occurred into a chronic subdural hematoma.
Presentation varies widely in acute subdural hematoma. Many of these patients are comatose on admission. However, approximately 50% of patients with head injuries who require emergency neurosurgery present with head injuries that are classified as moderate or mild (Glasgow Coma Scale) scores 9-13 and 14-15, respectively). Many of these patients harbor intracranial mass lesions.
In a large series of patients who developed intracranial hematomas requiring emergent decompression, more than half had lucid intervals and were able to make conversation between the time of their injury and subsequent deterioration. In a more comprehensive review of the literature on the surgical treatment of acute subdural hematomas, lucid intervals were noted in up to 38% of cases.
These patients may be more likely to benefit from medical and surgical intervention when instituted in a timely fashion (i.e., before further neurological deterioration).
Acute subdural hematoma is commonly associated with extensive primary brain injury. In one study, 82% of comatose patients with acute subdural hematomas had parenchymal contusions. The severity of the diffuse parenchymal injury shows a strong inverse correlation with the outcome of the patient.
In recognition of this fact, a subdural hematoma that is not associated with an underlying brain injury is sometimes termed a simple or pure subdural hematoma. The term complicated has been applied to subdural hematomas in which a significant injury of the underlying brain has also been identified.
Acute subdural hematoma is the most common type of traumatic intracranial hematoma, occurring in 24% of patients who present comatose. This type of head injury also is strongly associated with delayed brain damage, later demonstrated on CT scan. Such presentations portend devastating outcomes, and overall mortality rates are usually quoted at around 60%.
Significant trauma is not the only cause of subdural hematoma. Chronic subdural hematoma can occur in the elderly after apparently insignificant head trauma. Often, the antecedent event is never recognized. Chronic subdural hematoma is a common treatable cause of dementia. A minority of chronic subdural hematoma cases derived from acute subdural hematomas that have matured (i.e., liquefied) because of lack of treatment.
Pathophysiology
The usual mechanism that produces an acute subdural hematoma is a high-speed impact to the skull. This causes brain tissue to accelerate or decelerate relative to the fixed dural structures, tearing blood vessels.
Often, the torn blood vessel is a vein that connects the cortical surface of the brain to a dural sinus (termed a bridging vein). In elderly persons, the bridging veins may already be stretched because of brain atrophy (shrinkage that occurs with age).
Alternatively, a cortical vessel, either a vein or small artery, can be damaged by direct injury or laceration. An acute subdural hematoma due to a ruptured cortical artery may be associated with only minor head injury, possibly without an associated cerebral contusion. In one study, the ruptured cortical arteries were found to be located around the sylvian fissure.
The head trauma may also cause associated brain hematomas or contusions, subarachnoid hemorrhage, and diffuse axonal injury. Secondary brain injuries may include edema, infarction, secondary hemorrhage, and brain herniation.
Typically, low-pressure venous bleeding from bridging veins dissects the arachnoid away from the dura, and the blood layers out along the cerebral convexity. Cerebral injury results from direct pressure, increased intracranial pressure (ICP), or associated intraparenchymal insults.
In the subacute phase, the clotted blood liquefies. Occasionally, the cellular elements layer can appear on CT imaging as a hematocrit-like effect. In the chronic phase, cellular elements have disintegrated, and a collection of serous fluid remains in the subdural space. In rare cases, calcification develops.
Less common causes of subdural hematoma involve coagulopathies and ruptured intracranial aneurysms. Subdural hematomas have even been reported to be caused by intracranial tumors.
It has been asserted that the primary brain injury associated with subdural hematoma plays a major role in mortality. However, most subdural hematomas are thought to result from torn bridging veins, as judged by surgery or autopsy. Furthermore, not all subdural hematomas are associated with diffuse parenchymal injury. As mentioned earlier, many patients who sustain these lesions are lucid before their condition deteriorates – an unlikely scenario in patients who sustain diffuse damage.
Acute subdural hematoma
Investigation of brain physiological and biochemical parameters in patients with acute traumatic subdural hematoma has suggested variables that might be associated with secondary injury to the brain.
In a study of brain biochemical patterns after acute subdural hematoma evacuation, Hlatky et al. found that postsurgical patients who succumbed to their injury exhibited lower values of brain tissue oxygen tension and higher dialysate values of lactate and pyruvate in the brain underlying the hematoma. They suggested that identification of this brain biochemistry pattern after surgery might signify an evolving brain injury that warrants further evaluation or treatment.
Cerebral blood flow (CBF) can become markedly reduced. Schroder et al. reported that in 2 patients with acute subdural hematoma requiring emergent craniotomy, the hemisphere ipsilateral to the subdural hematoma demonstrated lower CBF than the contralateral hemisphere. Furthermore, CBF in both hemispheres was lower than normal.
Impressive increases in CBF and cerebral blood volume (CBV) that could not be attributed to pCO2 or blood pressure changes were noted immediately after surgery. The authors speculated that the decreased CBV caused by the subdural hematoma was a result of a compressed microcirculation, which was caused by increased ICP.
Herniation
Like other masses that expand within the skull, subdural hematomas may become lethal by increasing pressure within the brain, leading to pathologic shifts of brain tissue (brain herniations). Two common types of brain herniation are subfalcial (cingulate gyrus) herniation and transtentorial (uncal) herniation.
Subfalcial herniation may cause a cerebral infarct via compression of the anterior cerebral artery, and transtentorial herniation may cause an infarct via compression of the posterior cerebral artery. Transtentorial herniation is also associated with pressure on the third cranial nerve, causing decreased reactivity and then dilation of the ipsilateral pupil.
With progressive transtentorial herniation, pressure on the brainstem causes its downward migration. This tears critical blood vessels that supply the brainstem, resulting in Duret hemorrhages and death. Increased ICP may also decrease cerebral flood flow, possibly causing ischemia and edema; this further increases the ICP, causing a vicious circle of pathophysiologic events.
Chronic subdural hematoma
Chronic subdural hematoma is commonly associated with cerebral atrophy. Cortical bridging veins are thought to be under greater tension as the brain gradually shrinks from the skull; even minor trauma may cause one of these veins to tear. Slow bleeding from the low-pressure venous system often enables large hematomas to form before clinical signs appear.
Small subdural hematomas often spontaneously resorb. Larger collections of subdural blood usually organize and form vascular membranes that encapsulate the subdural hematoma. Repeated bleeding from small, friable vessels within these membranes may account for the expansion of some chronic subdural hematomas.
Chronic subdural hematomas may also evolve from the liquefaction of an acute subdural hematoma, particularly one that is relatively asymptomatic. Liquefaction usually occurs after 1-3 weeks, with the hematoma appearing hypodense on a CT scan.
Some chronic subdural hematomas may also enlarge from an osmotic gradient, drawing more fluid into the subdural space, or through the separate mechanism of calcification.
As a subdural hematoma expands in the subdural space, it raises the ICP and deforms the brain. The rise in ICP is initially compensated by efflux of cerebrospinal fluid (CSF) toward the spinal axis and compression of the venous system, expediting venous drainage through the jugular veins. During this stage, ICP rises relatively slowly, because the intracranial compliance is relatively high; in other words, the initial changes in intracranial volume are associated with small changes in ICP.
However, as the hematoma (and edema from associated parenchymal injury) expands, a limit is reached beyond which compensatory mechanisms fail. The intracranial compliance begins to decrease; small increases in intracranial volume are associated with larger increases in ICP. The ICP rises exponentially, leading to decreased cerebral perfusion and global cerebral ischemia. In a rapidly expanding hematoma, this whole process can happen in minutes.
In patients with chronic subdural hematoma, blood flow to the thalamus and basal ganglia regions appears to be particularly affected compared to that to the rest of the brain. Tanaka et al. suggested that impaired thalamic function can lead to a spreading depression that impairs various cortical regions, thereby producing various clinical deficits. They found that a 7% decrease of CBF was commonly associated with headache, whereas a 35% decrease of CBF was associated with neurological deficit such as hemiparesis.
Given that the pathophysiology of chronic subdural hematoma is often directly associated with cerebral atrophy, the fact that subdural hematomas are associated with conditions that cause cerebral atrophy (e.g., alcoholism, dementia) is not surprising. In a series reported by Foelholm and Waltimo, alcoholics constituted over half of the patient population. Most chronic subdural hematomas are probably caused by head injury; other causes and predisposing factors include coagulopathy, use of anticoagulants (including aspirin), seizure disorders, and CSF shunts.
Herniation syndromes
In addition to increasing the ICP, the hematoma deforms and displaces the brain. Eventually, transtentorial or subfalcine herniation can develop as the brain is pushed past the dural folds of the tentorial incisura or falx, respectively.
Tonsillar herniation through the foramen magnum may develop if the whole brain stem is forced down through the tentorial incisura by elevated supratentorial pressure. Although much less common than supratentorial subdural hematoma, infratentorial subdural hematoma can develop and cause tonsillar herniation and brainstem compression.
Characteristic herniation syndromes may develop as the brain shifts. As the medial temporal lobe, or uncus, herniates past the tentorium, it can compress the ipsilateral posterior cerebral artery, oculomotor nerve, and cerebral peduncle. Clinically, the consequent oculomotor nerve palsy and cerebral peduncle compression are often manifested by an ipsilaterally dilated pupil and a contralateral hemiparesis.
The patient also may develop a stroke of the posterior cerebral artery distribution. In approximately 5% of cases, the hemiparesis may be ipsilateral to the dilated pupil. This phenomenon is called the Kernohan notch syndrome and results when uncal herniation forces the midbrain to shift so that the contralateral cerebral peduncle is forced against the contralateral tentorial incisura.
Subfalcine herniation caused by midline brain shift may result in compression of anterior cerebral artery branches against the fixed falx cerebri, leading to infarcts in an anterior cerebral artery distribution.
Spontaneous subdural hematoma
Spontaneous subdural hematoma is rare. The literature is limited to sporadic case reports. These cases often have an arterial source; they are usually associated with the same pathology as that involved in subarachnoid or intracerebral hemorrhage. The blood from a ruptured aneurysm may dissect through the brain parenchyma or subarachnoid space into the subdural space.
Likewise, the blood released from a “hypertensive” intracerebral hemorrhage can dissect into the subdural space. In fact, a case has been reported of an acute spontaneous subdural hematoma precipitated by cocaine abuse.
Coagulopathy, occasionally associated with malignancy, also has been associated with spontaneous subdural hematoma. Subdural hematoma also can be caused by bleeding from intracranial tumors. The treatment of spontaneous subdural hematoma is similar to subdural hematoma caused by trauma, but the underlying cause must be sought and treated.
Subdural hygroma
Some chronic subdural hematomas may be derived from subdural hygromas. Brain atrophy or loss of brain tissue due to any cause, such as alcoholism, or stroke, may provide either an increased space between the dura and the brain surface where a subdural hygroma can form (see the image below) or traction on bridging veins that span the gap between the cortical surface and dura or venous sinuses.
Atrophy of the brain, resulting in a space between the brain surface and the skull, increases the risk of subdural hematoma (SDH).
Hygromas probably form after a tear in the arachnoid allows CSF to collect in the subdural space. A subdural hygroma may therefore also occur after head trauma; they are frequently asymptomatic.
Etiology
Causes of acute subdural hematoma include the following:
- Head trauma
- Coagulopathy or medical anticoagulation (e.g., warfarin [Coumadin], heparin, hemophilia, liver disease, thrombocytopenia)
- Nontraumatic intracranial hemorrhage due to cerebral aneurysm, arteriovenous malformation, or tumor (meningioma or dural metastases)
- Postsurgical (craniotomy, CSF shunting)
- Intracranial hypotension (e.g., after lumbar puncture, lumbar CSF leak, lumboperitoneal shunt, spinal epidural anesthesia
- Child abuse or shaken baby syndrome (in the pediatric age group)
- Spontaneous or unknown (rare)
Causes of chronic subdural hematoma include the following:
- Head trauma (may be relatively mild, e.g., in older individuals with cerebral atrophy)
- Acute subdural hematoma, with or without surgical intervention
- Spontaneous or idiopathic
Risk factors for chronic subdural hematoma include the following:
- Chronic alcoholism
- Epilepsy
- Coagulopathy
- Arachnoid cysts
- Anticoagulant therapy (including aspirin)
- Cardiovascular disease (e.g., hypertension, arteriosclerosis)
- Thrombocytopenia
- Diabetes mellitus
- In younger patients, alcoholism, thrombocytopenia, coagulation disorders, and oral anticoagulant therapy have been found to be more prevalent. Arachnoid cysts are more commonly associated with chronic subdural hematoma in patients younger than 40 years.
- In older patients, cardiovascular disease and arterial hypertension are found to be more prevalent. In one study, 16% of patients with chronic subdural hematomas were on aspirin therapy. Major dehydration is a less commonly associated condition and is found concurrently in only 2% of patients.
Epidemiology
Mortality/Morbidity
Acute subdural hematomas have been reported to occur in 5-25% of patients with severe head injuries, depending on the study. The annual incidence of chronic subdural hematoma has been reported to be 1-5.3 cases per 100,000 population. More recent studies have shown a higher incidence, probably because of better imaging techniques.
Sex- and age-related differences in incidence
Overall, subdural hematomas are more common in men than in women, with a male-to-female ratio of approximately 3:1. Men also have a higher incidence of chronic subdural hematoma. The male-to-female ratio has been reported to be 2:1.
The incidence of chronic subdural hematoma appears to be highest in the fifth through seventh decades of life. One retrospective study reported that 56% of cases were in patients in their fifth and sixth decades; another study noted that more than half of all cases were seen in patients older than 60 years. The highest incidence, 7.35 cases per 100,000 population, occurs in adults aged 70-79 years.
Adhesions existing in the subdural space are absent at birth and develop with aging; therefore, bilateral subdural hematomas are more common in infants. Interhemispheric subdural hematomas are often associated with child abuse.
Prognosis
The mortality associated with acute subdural hematoma has been reported to range from 36-79%. Many survivors do not regain previous levels of functioning, especially after an acute subdural hematoma severe enough to require surgical drainage. Favorable outcome rates after acute subdural hematoma range from 14-40%.
Several series have shown an increase in favorable outcome in younger patients.Age younger than 40 years was associated with a mortality rate of 20%, whereas age 40-80 years was associated with a mortality rate of 65%. Age older than 80 years carried a mortality rate of 88%.
Ultimate prognosis is related to the amount of associated direct brain damage and the damage resulting from the mass effect of the hematoma. Simple acute subdural hematoma (i.e., without parenchymal injury) accounts for about half of all cases and is associated with a mortality rate of about 20%. Complicated subdural hematoma (e.g., with accompanying contusion or laceration of a cerebral hemisphere) is associated with a mortality rate of about 60%.
Findings on CT scan or MRI may help indicate prognosis. Such findings may include the following:
- Thickness or volume of the hematoma
- Degree of midline shift
- Presence of associated traumatic intraparenchymal lesions
- Compression of the brainstem or basal cisterns
The first CT scan may underestimate the size of parenchymal contusions.
In general, a poor preoperative neurologic status may be a harbinger of a poor outcome. In addition to factors discussed above, poor prognostic indicators for acute subdural hematoma have been reported to include the following:
- Low initial (< 8) and post-resuscitation (< 8) Glasgow coma scale
- Low Glasgow coma scale motor score on admission (< 5)
- Pupillary abnormalities
- Alcohol use
- Injury by motorcycle accident
- Ischemic damage
- Hypoxia or hypotension
- Difficulty in controlling ICP
Elevated ICP postoperatively indicates a poor prognosis and may indicate the severity of the underlying brain injury (e.g., trauma, secondary infarction).
In a retrospective review of 109 consecutive patients with head injury with a CT scan diagnosis of acute traumatic subdural hematoma, Phuenpathom et al found that poor outcome was strongly correlated with the best sum GCS score within the first 24 hours of head injury and pupillary inequality. Age and pupillary reaction to light also correlated well with the outcome.
The mortality in the whole series was 50%, and mortality for all 37 patients with a GCS score of 3 was 100% (this rate decreased as the GCS increased). The mortality for those with unequal pupils was 64%, versus 40% for those with equal pupils. The mortality associated with one nonreactive pupil was 48%, versus 88% with bilateral nonreactive pupils. The outcome status of the patients with bilateral nonreactive pupils who survived was not noted.
Wilberger et al. also found an 88% mortality associated with fixed, dilated pupils and noted a 7% functional recovery in survivors with this finding. This study found that neurologic presentation and postoperative ICP (which was not evaluated by Phenpatham et al.) were strong predictors of outcome. Wilberger et al. also found a trend of increasing mortality rate with age, although it was not statistically significant.
A review by Sakas et al. of 1-year outcomes following craniotomy for traumatic hematomas in patients with fixed, dilated pupils suggested that the presence of an acute subdural hematoma was the single most important predictor of a negative outcome. Patients with subdural hematomas had a mortality of 64%, compared with a mortality of 18% in patients with extradural hematomas.
Seelig et al. also showed that neurologic examination findings and postoperative ICP were important prognostic factors. The peak ICP was less than 20 mm Hg in 53% of patients with acute traumatic subdural hematoma (similar to 59% of patients with other types of head injuries), but this group accounted for 79% of the patients with functional recoveries.
All patients with uncontrollably elevated ICP (>60 mm Hg) died. These authors claimed a 25% functional recovery rate (defined by the Glasgow Outcome Scale) in patients presenting with fixed, dilated pupils.
Acute subdural hematomas that would otherwise be considered operative by imaging criteria may resolve on their own, although this is rare. A series of 4 such patients was reported by Kapsalaki et al.
No clear prognostic factors are associated with chronic subdural hematoma. While some authors have found an association with preoperative level of neurological function and outcome, others have not. Early diagnosis before significant neurologic deterioration may correlate with a more favorable prognosis. No correlation has been found between preoperative CT scan findings and postoperative outcome.
The mortality within 30 days of surgery is 3.2-6.5%. Eighty percent of patients resume their pre-hematoma level of function. Sixty-one percent of patients aged 60 years or younger and in 76% of patients older than 60 years have favorable outcomes. In a relatively recent series, 89.4% of patients with chronic SDH who were treated with a closed drainage system had a good recovery and 2.2% worsened.
Mori et al. found that old age, pre-existing cerebral infarction, and subdural air after surgery correlated with poor brain expansion.Stanisic et al. reported a 14.9% postoperative recurrence rate; various factors were associated with this.
The morbidity and mortality rates associated with surgical treatment of chronic subdural hematoma have been estimated at 11% and 5%, respectively. Between 86% and 90% of patients with chronic subdural hematoma are adequately treated after one surgical procedure.
History
Acute traumatic subdural hematoma often results from falls, violence, or motor vehicle accidents. Suspect acute subdural hematoma whenever the patient has experienced moderately severe to severe blunt head trauma. The clinical presentation depends on the location of the lesion and the rate at which it develops. Often, patients are rendered comatose at the time of the injury. A subset of patients remains conscious; others deteriorate in a delayed fashion as the hematoma expands.
Patients found to have an acute subdural hematoma are usually older than other patients with trauma. In one study, the average age of a patient with trauma but without acute subdural hematoma was 26 years, while the average age of patients with an acute subdural hematoma was 41 years. Therefore, older patients appear to be at greater risk for developing an acute subdural hematoma after head injury. This is believed to stem from older patients having more brain atrophy, which allows more shear force against bridging veins immediately after impact.
Subacute subdural hematomas are defined arbitrarily as those that present between 4 and 21 days after injury. Chronic subdural hematomas are arbitrarily defined as those hematomas presenting 21 days or more after injury. These numbers are not absolute, and a more accurate classification of a subdural hematoma usually is based on imaging characteristics.
Chronic subdural hematoma
One quarter to one half of patients with chronic subdural hematoma have no identifiable history of head trauma. If a patient does have a history of head trauma, it is usually mild.
Of patients who have sustained head injury, symptoms develop after 1-4 weeks in 25%. Another 25% experience symptoms from 5 weeks to 3 months before their hospital admission. Only one third of patients have no asymptomatic period.
Clinical presentation for chronic subdural hematoma is often insidious, with symptoms that include the following:
- Decreased level of consciousness
- Headache
- Difficulty with gait or balance
- Cognitive dysfunction or memory loss
- Personality change
- Motor deficit (e.g., hemiparesis)
- Aphasia
Chronic subdural hematoma may have a presentation similar to Parkinson disease. An acute presentation is also possible, as in the case of a patient who presents with a seizure.
Headache and confusion appear to be the most common presenting features, occurring in as many as 90% and 56% of cases, respectively. In 75% of cases, the headache had at least one of the following characteristics:
- Sudden onset
- Severe pain
- Accompanying nausea and vomiting
- Exacerbation by coughing, straining, or exercise
Other common symptoms include weakness, seizures, and incontinence.
Hemiparesis and decreased level of consciousness are common, occurring in approximately 58% and 40%, respectively. Hemiparesis was ipsilateral to the hematoma in 40% of cases in one series. Gait dysfunction is another common finding.
When signs of chronic subdural hematoma in different age groups are compared, somnolence, confusion, and memory loss are significantly more common in elderly patients (aged 60-79 y). Signs of increased intracranial pressure (ICP), such as headache and vomiting, are more likely to be seen in younger patients. Fluctuating signs or symptoms occur in as many as 24% of cases.
Risk factors
Any degree or type of coagulopathy should heighten suspicion of subdural hematoma. Hemophiliacs can develop subdural hematoma after seemingly trivial head trauma. An aggressive approach to diagnosis and immediate correction of the factor deficiency to 100% activity is paramount.
Alcoholics are prone to thrombocytopenia, prolonged bleeding times, and blunt head trauma. Maintain a high level of suspicion in this population. Promptly obtain a computed tomography (CT) scan of the head when the degree of trauma is severe, focal neurologic signs are noted, or intoxication does not resolve as anticipated. In alcoholics, more than any other cohort, acute or chronic subdural hematomas can be due to the deadly combination of repetitive trauma and alcohol-associated coagulopathies.
Patients on anticoagulants can develop subdural hematoma with minimal trauma and warrant a lowered threshold for obtaining a head CT scan.
Physical Examination
Physical examination of patients with head trauma should emphasize assessment of neurologic status using the Glasgow Coma Scale (GCS). The initial neurologic examination provides an important baseline that should be used to follow the patient’s clinical course. When recorded in the form of the GCS score, it also provides important prognostic information.
Patients with serious head injuries often are intubated quickly and given trauma-oriented care. However, because of its prognostic significance, a brief neurologic examination quantified by using the GCS is an essential component of the secondary assessment and takes less than 2 minutes to complete. The GCS focuses on the patient’s ability to produce intelligible speech, open the eyes, and follow commands. During the initial evaluation, the patient should be assessed for the ability to open the eyes spontaneously or in response to voice or to pain.
The patient’s speech and mentation should be characterized as oriented, confused, inappropriate, incomprehensible, or none. The patient’s motor function is determined by the patient’s ability to follow commands on both the left and right sides. If the patient is unable to follow commands, note his or her ability to localize painful stimuli or to exhibit normal flexion on either side in response to the pain.
Decorticate and decerebrate posturing or lack of any motor function should also be recorded. Assess the size and reactivity of both pupils. Signs of external trauma should alert the physician to the expected location of coup or contrecoup injuries on CT scan.
A GCS score less than 15 after blunt head trauma in a patient with no intoxicating substance use (or impaired mental status baseline) warrants consideration of an urgent CT scan. Search for any focal neurologic deficits or signs of increased ICP. Any abnormality of mental status that cannot be explained completely by alcohol intoxication or the presence of another mind-altering substance should increase suspicion of subdural hematoma in the patient with blunt head trauma.
The presence of a focal neurologic sign following blunt head trauma is ominous and requires an emergent explanation. Patients with possible subdural hematoma should be examined for related injuries (using guidelines established by the American College of Surgeons Committee on Trauma), such as cervical spine fracture, spinal cord injury, or long-bone fractures.
The clinical presentation of a patient with an acute subdural hematoma depends on the size of the hematoma and the degree of any associated parenchymal brain injury. Symptoms associated with acute subdural hematoma include the following:
- Headache
- Nausea
- Confusion
- Personality change
- Decreased level of consciousness
- Speech difficulties
- Other change in mental status
- Impaired vision or double vision
- Weakness
Of course, such symptoms could also be caused by other conditions.
Neurologic findings associated with acute subdural hematoma may include the following:
- Altered level of consciousness
- A dilated or nonreactive pupil ipsilateral to the hematoma (or earlier, a pupil with a more limited range of reaction)
- Hemiparesis contralateral to the hematoma
A host of findings could be associated with these, such as brisk or abnormal reflexes, aphasia (usually with a left-sided hematoma), upper-extremity drift, or impairment of cortical sensory function. Less common findings include papilledema and unilateral or bilateral cranial nerve VI palsy. Some of the above may occur later in the clinical course; for instance, coma with a dilated fixed pupil usually indicates unilateral transtentorial herniation. Lack of a finding (e.g., papilledema) cannot rule out subdural hematoma.
Less commonly, the hemiparesis may be ipsilateral to the hematoma, possibly due to direct parenchymal injury or compression of the cerebral peduncle contralateral to the hematoma against the edge of the tentorium cerebelli (the Kernohan notch phenomenon). Therefore, if the findings are conflicting, the most reliable indicator (by examination) of the side of the hematoma is a dilated or nonreactive pupil, which appears on the same side as the hematoma.
Patients may have a lucid interval after developing a traumatic subdural hematoma. In addition, initial CT scan findings may be negative (i.e., delayed intracranial hemorrhage).
Acute subdural hematomas most often occur over the cerebral hemispheres (convexity). However, they may also be found between the hemispheres along the falx (interhemispheric subdural hematoma), along the tentorium, or in the posterior fossa.
Interhemispheric subdural hematomas may be asymptomatic or manifest as headache,impaired consciousness, or hemiparesis or monoparesis (more likely to affect the contralateral leg than arm). Interhemispheric subdurals are usually managed conservatively unless neurologic deterioration is found.
Look for signs of a basilar skull fracture. These include bilateral periorbital ecchymoses (raccoon eyes) and retroauricular ecchymoses (Battle sign). Note the presence or absence of cerebrospinal (CSF) rhinorrhea or otorrhea.
Areas surrounding lacerations should be shaved and inspected. Patients with severe head injuries should be assumed to have a cervical spine (C-spine) injury; immobilize the patient until clinical and radiographic studies can prove otherwise.
Chronic subdural hematoma
Neurologic examination for chronic subdural hematoma may demonstrate any of the following:
- Mental status changes
- Papilledema
- Hyperreflexia or reflex asymmetry
- Hemianopsia
- Hemiparesis
- Third or sixth cranial nerve dysfunction
Such findings may also be associated with other entities. In patients aged 60 years or older, hemiparesis and reflex asymmetry are common presenting signs. In patients younger than 60 years, headache is a common presenting symptom.
Chronic subdural hematomas have been reported to be bilateral in 8.7-32% of cases.
Diagnostic Considerations
The differential diagnosis of an acute traumatic subdural hematoma is the same as that for any traumatic, intracranial mass lesion. This includes intracerebral hematoma and contusion.
Because of its variable course and presentation, including the frequent lack of a history of head trauma, as many as 72% of cases of chronic subdural hematoma were misdiagnosed in the pre–computed tomography (CT) era. Prior to the availability of CT, common misdiagnoses included the following:
- Dementia
- Stroke
- Transient ischemic attack
- Tumor
- Subarachnoid hemorrhage
- Meningitis
- Encephalitis
Differential Diagnoses
- Child Abuse
- Elder Abuse
- Emergent Management of Subarachnoid Hemorrhage
- Epidural Hematoma in Emergency Medicine
- Hemorrhagic Shock in Emergency Medicine
- Ischemic Stroke in Emergency Medicine
- Meningitis
Approach Considerations
An emergent computed tomography (CT) scan of the head needs to be performed when an acute subdural hematoma is suspected. It should be obtained immediately after the patient is stabilized using standard Advanced Trauma Life Support (ATLS) guidelines. CT scanning is also the initial imaging modality of choice for chronic subdural hematoma.
The trauma team and neurosurgeon must determine quickly which lesions warrant immediate evacuation, and CT is the imaging modality of choice to facilitate this decision. Modern CT devices can produce appropriate images in about 5 minutes, and the scans are highly sensitive to acute blood. Although magnetic resonance imaging (MRI) is superior for demonstrating the size of an acute subdural hematoma and its effect on the brain, noncontrast head CT is the primary means of making a diagnosis and suffices for immediate management purposes.
A worsening of the Glasgow Coma Scale by 2 or more points should prompt repeat imaging in salvageable patients. A cervical spine radiograph series is important in evaluating the possibility of concomitant cervical spine fracture.
- Initial blood tests include the following:
- Complete blood count
- Hemoglobin or hematocrit
- Coagulation profile
- Basic metabolic panel
- Type and screen/crossmatch
In addition, drug and alcohol screenings may be important for correlating the neurologic examination with the imaging studies.
Detection of electrolyte abnormalities is important because they can exacerbate brain injury and therefore require correction in a timely manner. For example, hyponatremia (5-12% estimated incidence in patients with head injury) can potentiate brain edema and cause seizures.
Coagulation Profile
Coagulation profiles are particularly important for patients taking anticoagulants and for alcoholics, who may have an associated coagulopathy placing them at high risk for subdural hematoma. Their altered mental status may be from the hematoma rather than ethanol.
In addition, the prevalence of coagulation abnormalities has long been recognized as unusually high in patients with head injuries. These abnormalities are believed to result from the release of thromboplastic materials by damaged brain tissue.
Stein et al. showed that the presence of coagulopathy and the development of delayed brain injury are strongly associated. In a review of 253 patients with head injury who required serial CT scans, the risk of developing a delayed brain insult as seen on CT scan increased from 31% in patients with coagulation study findings within reference range to almost 85% in patients with abnormal findings on prothrombin time (PT), activated partial thromboplastin time (aPTT), or platelet count.
Subdural hematomas themselves were associated with disease progression; 26 of 35 patients with subdural hematoma had expansion of their hematoma or a delayed brain injury seen on a follow-up CT scan. Therefore, all patients with head injury should have at least a basic coagulation panel (PT, aPTT, and platelet count). Fresh frozen plasma or platelets should be given as needed. However, awaiting the results of these studies should not delay emergency surgery.
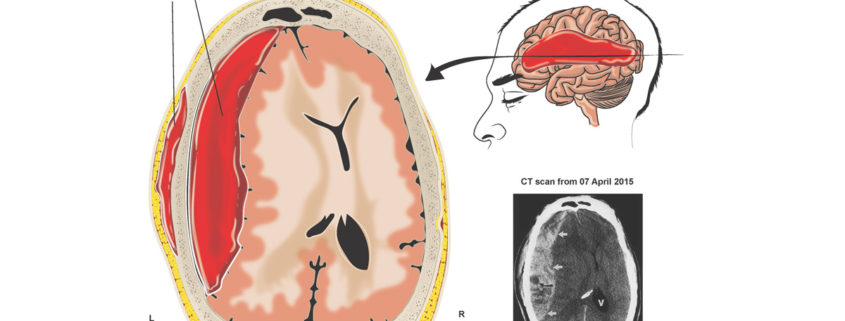
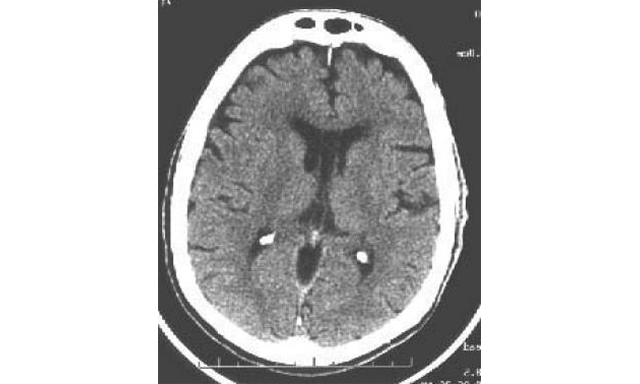
Computed Tomography
On non-contrast CT scan, an acute subdural hematoma appears as a hyperdense (white), crescent-shaped mass between the inner table of the skull and the surface of the cerebral hemisphere (see the images below). Subdural hematomas are concave toward the brain and unlimited by suture lines, as opposed to epidural hematomas, which are convex toward the brain and restricted by suture lines. Rarely, a subdural hematoma appears lens shaped (i.e., more like an epidural hematoma). Acute subdural hematomas are usually unilateral.
Acute right-sided subdural hematoma associated with significant midline shift (i.e., subfalcine herniation) shown on CT scan.
An acute subdural hematoma (SDH) as a complication of a craniotomy. Note the significant mass effect with midline shift.
Acute subdural hematomas occur most commonly over the cerebral convexity in the parietal region (see the image below). The second most common site is above the tentorium cerebelli.
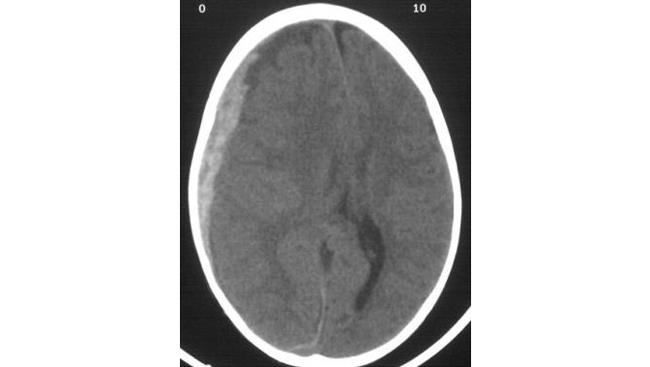
Acute subdural hematoma. Note the bright (white) image properties of the blood on this non-contrast cranial CT scan. Note also the midline shift. Image courtesy of J. Stephen Huff, MD
Subdural hematomas are relatively uncommon in the posterior fossa since the cerebellum undergoes little movement, which is protective of its bridging cortical veins. Subdural hematomas that do occur in that location are usually a result of parenchymal cerebellar injury.
A small acute subdural hematoma may be difficult to appreciate because of the appearance of the overlying skull. Use of the bone window setting may aid in discrimination.
A subdural hematoma may also be located along the falx cerebri (i.e., interhemispheric), along the tentorium, or in the posterior fossa. Interhemispheric subdural hematoma causes the falx cerebri to appear thickened and irregular and often is associated with child abuse.
All or part of an acute subdural hematoma may appear hypodense or isodense to brain if the patient’s hematocrit is low, if the clot is hyperacute (e.g., < 1 hour old), if the subdural space contains active bleeding, if coagulopathy is present, or if the CSF is creating a dilutional effect.
Detection of an isodense subdural hematoma may require a high index of suspicion; subtle changes in the appearance or position of the cortical sulci may be found. Contrast-enhanced CT or MRI may help to better define the lesion. Interestingly, isodense subdural hematomas may be either hypointense or hyperintense on T2-weighted MRI; this may be a clue to the underlying pathophysiology.
Some degree of midline shift should be present with moderate or large subdural hematomas. Suspect a contralateral mass when midline shift is absent. If midline shift seems excessive, suspect underlying cerebral edema.
CT in subacute subdural hematoma
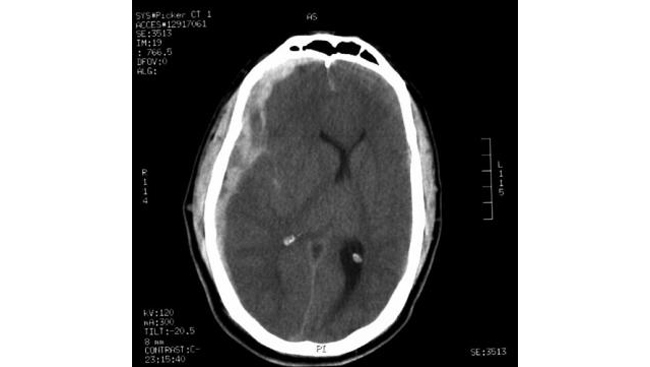
In the second and third weeks (the subacute phase), subdural hematomas become isodense (with respect to the brain) and more difficult to appreciate on a noncontrast head CT scan (see the images below). Also, subacute subdural hematomas often become lens-shaped and can be confused with an epidural hematoma.
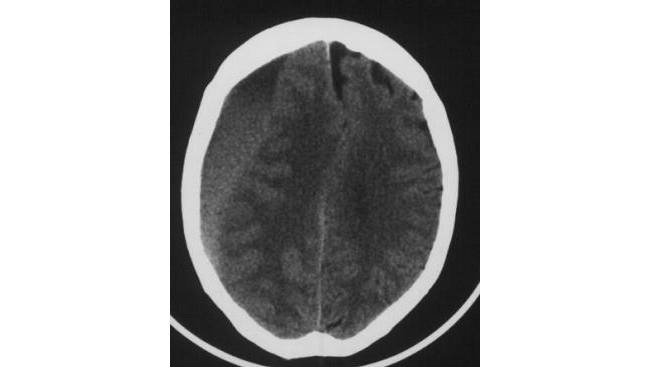
Subacute subdural hematoma. The crescent-shaped clot is less white than on CT scan of acute subdural hematoma. In spite of the large clot volume, this patient was awake and ambulatory. Image courtesy of J. Stephen Huff, MD.
An isodense subdural hematoma (SDH). Note that no sulcal markings are below the inner table of the skull on the right side. This hematoma has scattered areas of hyperdense, or acute, blood within it.
For this reason, either contrast-enhanced CT or MRI should be considered for imaging 48-72 hours after head injury. On contrast-enhanced CT scans, cortical veins over the cerebral surface are opacified and help delineate the lesion. On T1-weighted MR images, subacute lesions are hyperdense.
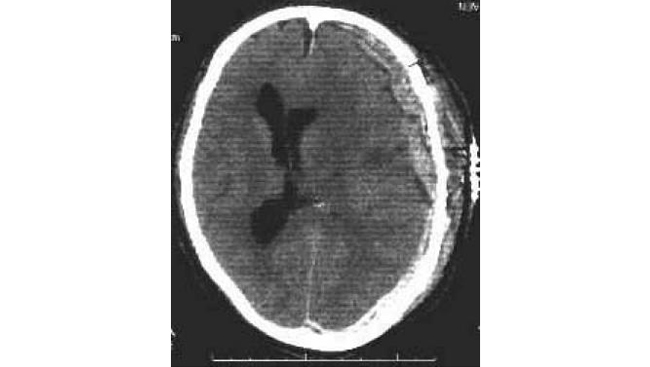
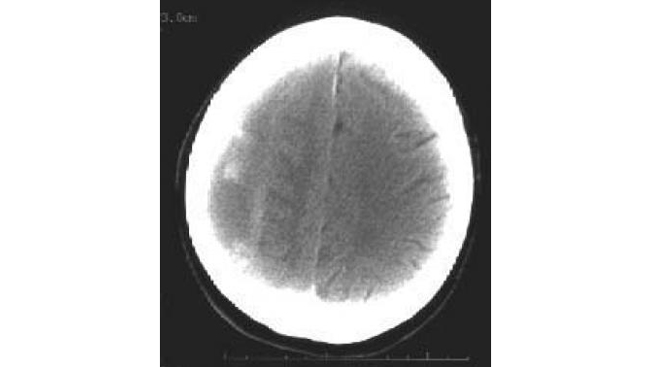
CT in chronic subdural hematoma
In the chronic phase, the lesion becomes hypodense and is easy to appreciate on a noncontrast head CT scan. About 20% of chronic subdural hematomas are bilateral, however, and this may prevent midline shift, thereby making the subdural hematoma harder to detect. See the image below. Despite this caveat, CT scan still supersedes MRI because of its reliability, shorter study time, and lower cost.
Bilateral chronic subdural hematomas shown on CT scan. Midline shift is absent because of bilateral mass effect. Subdural hematoma is bilateral in 20% of patients with chronic subdural hematoma.
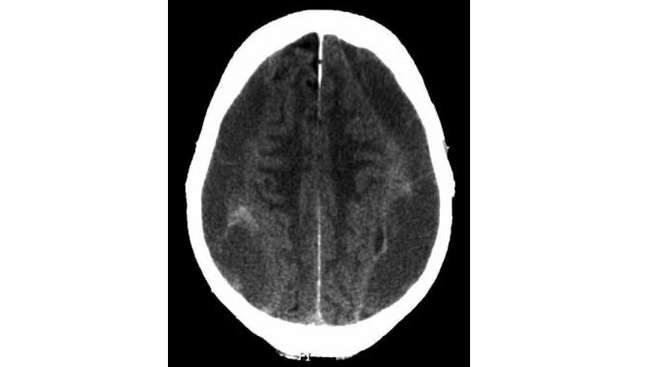
Often, a chronic subdural hematoma appears as a heterogeneously dense lesion indicative of recurrent bleeding with a fluid level between the acute (hyperdense) and chronic (hypodense) components of the hematoma (see the image below).
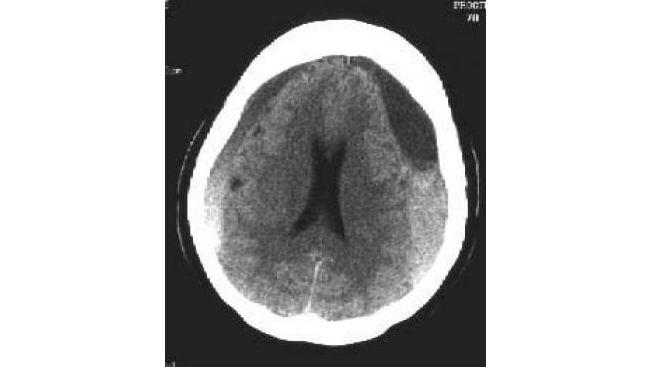
Chronic subdural hematomas (SDHs) are commonly bilateral and have areas of acute bleeding, which result in heterogeneous densities. Note the lack of midline shift due to the presence of bilateral hematomas.
On a contrast-enhanced CT scan, the chronic subdural hematoma membrane enhances to varying degrees, depending on numerous factors. Sometimes, a contrast-enhanced scan shows evidence of an underlying cause, such as a tumor or vascular lesion (eg, in patients with acute but nontraumatic subdural hematoma).
Although the distinction between subacute and chronic is an arbitrary one, it can be important. Chronic subdural hematomas have a liquid consistency, typically resembling crankcase oil, and can be drained through burr holes. The consistency of subacute subdural hematomas might be too thick for burr-hole drainage and might require craniotomy.
Other Studies
Magnetic resonance imaging
MRI is less useful than CT in diagnosing an acute subdural hematoma because of the increased time needed to obtain the study and the inability to use metallic objects that are needed to resuscitate patients with trauma (e.g., most ventilators) in the scanning environment.
MRI can be a useful study to evaluate associated parenchymal brain injury and predict prognosis, but only after stabilizing and treating any life-threatening lesions. MRI is more sensitive for detecting non-hemorrhagic brain lesions, contusions, and diffuse axonal injury.
An MRI is helpful in imaging chronic subdural hematoma when CT scans are difficult to interpret (e.g., when suspecting an isodense hematoma). MRI may be particularly helpful in diagnosing bilateral chronic subdural hematoma because a midline shift may not be apparent on CT scan.
Histologic findings
Acute subdural hematomas usually contain both liquid and clotted blood. Intact erythrocytes are usually found within the clot. Associated skull fractures and underlying focal traumatic parenchymal damage are often present.
Fibroblastic membranes form on the dural side and arachnoid side of the chronic subdural hematomas, with the duralneomembrane being more vascular. The neomembrane consists of many capillaries, intact and lysed erythrocytes, hemosiderin-laden macrophages, and granulation tissue.
Approach Considerations
As with any trauma patient, resuscitation begins with the ABCs (airway, breathing, circulation). All patients with a Glasgow Coma Scale (GCS) score of less than 8 should be intubated for airway protection.
Despite prompt surgical evacuation of hematomas, patients with acute subdural hematomas often have a poor prognosis because of associated underlying brain injury. Patients often require intensive care postoperatively for ventilator-dependent respiration, strict blood pressure control, and management of intracranial hypertension. The mechanism, exact pathophysiology, and optimal treatment for chronic subdural hematomas has still not been definitively determined. Further work in delineating why membranes form and how to prevent or reverse their formation may lead to improvements in treatment strategies.
When deciding whether to operate, consider the patient’s prognosis. The ideal is to maximize the likelihood of appropriate resource allocation and, more importantly, allow for appropriate family counseling; keep in mind that no method of assessing the prognosis is 100% accurate.
Consult a neurosurgeon as soon as the diagnosis is suspected and initiate transfer if another facility is required for diagnosis or management.
Chronic subdural hematoma
In patients who have no significant mass effect on imaging studies and no neurologic symptoms or signs except mild headache, chronic subdural hematomas have been observed with serial scans and have been seen to remain stable or to resolve.
Although hematoma resolution has been reported, it cannot be reliably predicted, and no medical therapy has been shown to be effective in expediting the resolution of acute or chronic subdural hematomas.
Surgical Decompression
Surgery for emergent decompression has been advocated if the acute subdural hematoma is associated with a midline shift greater than or equal to 5 mm. Surgery also has been recommended for acute subdural hematomas exceeding 1 cm in thickness. These indications have been incorporated into the Guidelines for the Surgical Management of Acute Subdural Hematomas proposed by a joint venture between the Brain Trauma Foundation and the Congress of Neurological Surgeons, released in 2006.
These guidelines also call for emergent decompression in a comatose patient with an acute subdural hematoma less than 1 cm in thickness causing a midline shift of less than 5 mm if any of the following criteria are met:
- The GCS score decreases by 2 or more points between the time of injury and hospital evaluation
- The patient presents with fixed and dilated pupils
- The intracranial pressure (ICP) exceeds 20 mm Hg
In a series of patients with acute traumatic subdural hematoma initially treated conservatively, Wong found that if patients presented with a GCS score of 15 or lower and a midline shift greater than 5 mm, their condition usually would deteriorate, and they would require surgery. In another series reported by Matthew et al., all patients initially treated nonoperatively who subsequently required surgery presented with subdural hematomas that were at least 10 mm thick on their initial CT scan.
Surgery has been advocated when a subdural hematoma is associated with compressed or effaced basilar cisterns. In one large series of patients with severe head injuries, the mortality rates were 77%, 39%, and 22% for patients with effaced, compressed, or normal cisterns, respectively.
A meta-analysis comparing the efficacy of various methods of chronic subdural hematoma evacuation supported twist drill craniostomy drainage at the bedside for patients who are high-risk surgical candidates with non-septated chronic subdural hematomas. Chronic subdural hematomas with significant membrane formation were most effectively treated with craniotomy.
A decision analysis performed by Lega et al. revealed that bur-hole craniostomy was the most efficient form of surgical drainage for uncomplicated chronic subdural hematomas. Intraoperative subdural irrigation or postoperative subdural drainage did not significantly affect treatment outcomes.
Preoperative Treatments
Although significant acute traumatic subdural hematoma requires surgical treatment, temporizing medical maneuvers can be used preoperatively to decrease intracranial pressure. These measures are germane for any acute mass lesion and have been standardized by the neurosurgical community. They are discussed only briefly.
Adequate respiration should be initially addressed and maintained to avoid hypoxia. The patient’s blood pressure should be maintained at normal or high levels using isotonic saline, pressors, or both. Hypoxia and hypotension, which are particularly detrimental in patients with head injury, are independent predictors of poor outcome.
Short-acting sedatives and paralytics should be used only when needed to facilitate adequate ventilation or when elevated intracranial pressure is suspected. If the patient exhibits signs of a herniation syndrome, administer mannitol 1 g/kg rapidly by intravenous (IV) push.
The patient should also be mildly hyperventilated (pCO2 30-35 mm Hg). Hyperventilation may decrease cerebral blood flow, thereby causing cerebral ischemia.
Administer anticonvulsants to prevent seizure-induced ischemia and subsequent surges in intracranial pressure. Do not give steroids, as they have been found to be ineffective in patients with head injury.
A patient with coagulopathy or a patient with an acute SDH who is receiving anticoagulant medication should be transfused with prothrombin complex concentrate, fresh frozen plasma (FFP), platelets, or both to maintain the prothrombin time (PT) within the reference range and the platelet count above 100,000. Heparin may need to be reversed with protamine; patients receiving warfarin are given vitamin K. Dabigatran can be reversed with idarucizumab, and other reversal agents for the novel anticoagulants are under investigation. In patients who are receiving therapeutic anticoagulation, the potential effects of reversing the anticoagulation need to be considered.
The use of other factors, such as recombinant activated factor VII (rFVIIa), is under investigation. With traumatic intracranial hemorrhage in patients taking warfarin, use of rFVIIa was associated with a decreased time to normal International Normalized Ratio (INR). However, no difference in mortality was identified. Use of rFVIIa in patients on warfarin requires further study to demonstrate improved clinical outcomes before being routinely incorporated into clinical care.
The use of sequential CT scanning is important. Although each patient must be treated individually, patients who have small acute SDHs thinner than 5 mm on axial computed tomography (CT) images without mass effect to cause midline shift or neurological signs have been observed clinically, with acceptable results (see the image below).
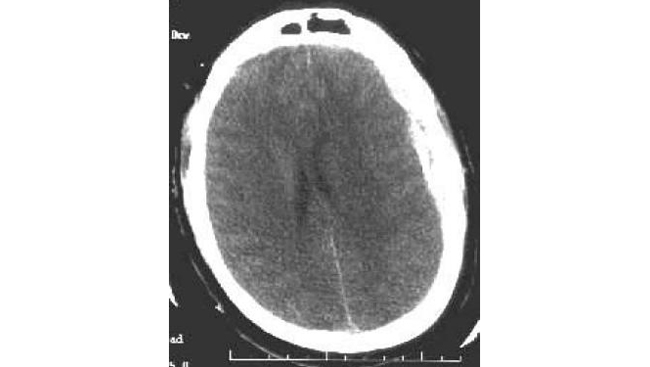
A left-sided acute subdural hematoma (SDH). Note the high signal density of acute blood and the (mild) midline shift of the ventricles.
Hematoma resolution should be documented with serial imaging because an acute subdural hematoma that is treated conservatively can evolve into a chronic hematoma. For serial imaging, magnetic resonance imaging (MRI) may be more sensitive, but CT may be more convenient and less expensive.
Medication Summary
Although significant acute traumatic subdural hematoma requires surgical treatment, temporizing medical maneuvers can be preoperatively used to decrease intracranial pressure. Short-acting sedatives and paralytics should be used only when needed to facilitate adequate ventilation or when elevated intracranial pressure is suspected. If the patient exhibits signs of a herniation syndrome, administer mannitol 1 g/kg rapidly by intravenous (IV) push.
Osmotic Diuretics
Class Summary
These agents may help reduce intracranial pressure.
Mannitol (Osmitrol)
Mannitol may reduce subarachnoid space pressure by creating an osmotic gradient between the cerebrospinal fluid in the arachnoid space and the plasma. It is not for long-term use. Initially assess for adequate renal function in adults by administering a test dose of 200 mg/kg, given IV over 3-5 min; this should produce urine flow of at least 30-50 mL/h of urine over 2-3 hours.