Top 5 Pitfalls in Managing Shock
Shock is a common condition that emergency department clinicians must be experts in treating. It is easy, however, to overlook the presence of shock in patients who initially look well or have seemingly normal systolic blood pressure (SBP), and the result can be deadly.
The following is a list of top 5 pitfalls in managing shock, based on 25 years of personal experience in clinical care and medical malpractice consultation work.
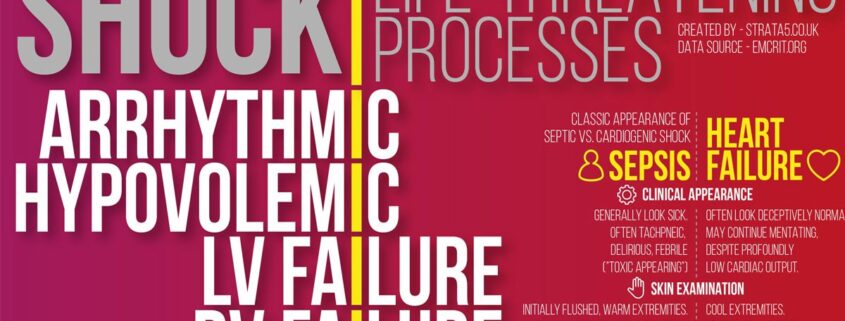
1. Failure to consider the differential diagnosis of shock
Shock has multiple causes, but it is easy to focus only on the most common ones, such as hypovolemia and sepsis, and forget about less common but critically important ones such as anaphylaxis and adrenal crisis. A useful mnemonic to remember the differential diagnosis of shock:
SHOCK’D:
- Septic, spinal (neurogenic)
- Hypovolemic, hemorrhagic
- Obstructive (pulmonary embolism, tension pneumothorax, tamponade)
- Cardiogenic, compartment syndrome (abdominal)
- K: Anaphyla’k’tic, endo’k’rine
- Drugs
Providers should always consider the full differential of the etiologies before settling on a diagnosis and treatment plan.
2. Overreliance on SBP rather than mean arterial pressure
It is important to remember that we live only one third of our life in systole but two thirds in diastole; therefore, diastolic blood pressure (DBP) in many respects is a better marker of vital organ perfusion than SBP. Mean arterial pressure (MAP) appropriately considers the importance of DBP:
MAP = (DBP x 2 + SBP)/3.
A nice example of the relative value of DBP versus SBP is in comparing a patient with a blood pressure of 90/60 mm Hg versus another patient at 110/40 mm Hg. Those who focus mostly on SBP would probably say that the second patient has a better blood pressure, but in fact, the first patient has better perfusion (MAP 70 mm Hg versus 63 mmHg, respectively).
Patient 1: (60 x 2 + 90)/3 = MAP 70
Patient 2: (40 x 2 + 110)/3 = MAP 63
Focus on DBP and MAP instead of just SBP!
3. Lackadaisical approach to treating shock
Shock needs to be treated aggressively and rapidly to avoid organ injury. Although it is appropriate in most cases to resuscitate patients with fluids, adequate intravenous (IV) fluid resuscitation can sometimes take some time. While awaiting a response to fluids, it is reasonable to initiate peripheral norepinephrine. Bai and colleagues demonstrated that for every hour delay in treating shock (with norepinephrine), the mortality increased by 5%. On the other hand, when norepinephrine was initiated within 2 hours of diagnosing septic shock, patients demonstrated improved lactate clearance, more rapid resolution of hypotension, and a resultant reduction in total duration of need for vasopressors. Peripheral norepinephrine can be transitioned to central administration, if still needed, during subsequent hours.
The key point here is that if patients are not responding rapidly to IV fluids, do not delay starting the norepinephrine.
4. Overzealous fluid administration
Not all patients in shock benefit from aggressive IV fluid administration. Patients with right ventricular dysfunction (e.g., patients with massive pulmonary emboli) can decompensate with large-volume resuscitation.
Instead, a bedside assessment of whether a patient will respond to fluids can be performed by way of a passive leg raise and via the use of bedside ultrasound (pulse pressure variation, inferior vena cava collapsibility, and so forth). These assessments can be repeated during the resuscitation and can help decide whether a patient will benefit most from fluids or vasopressors.
5. Failure to appreciate the shock index
The shock index (SI) is defined as the heart rate divided by the SBP. A normal value is < 0.7. An elevated SI > 0.7 in patients with infection is a strong predictor of systemic inflammatory response syndrome (SIRS), and a value ≥ 1 is a highly specific predictor of hyperlactatemia and 28-day mortality.
Other studies have corroborated the value of SI in patients with sepsis as a strong predictor of the need for vasopressor use, fluid responsiveness, organ failure, myocardial dysfunction, and mortality. SI has also been found to be helpful in the preintubation assessment of patients with impending respiratory failure.
Studies have reported that approximately 2% of ED intubations are associated with subsequent cardiac arrest, and an SI > 0.8-1.0 is a predictor of the postintubation arrest.
Therefore, clinicians are advised to assess the shock index prior to intubation, and when the SI is elevated, focus on hemodynamic resuscitation to the greatest extent possible prior to intubation. Furthermore, it is advisable to have vasopressors on hand in anticipation of possible hemodynamic collapse following the intubation.