Neurologic Disease and Pregnancy
As a consequence of the immense growth in therapeutic options for neurologic disorders over the past decade, when a woman becomes pregnant, the question is no longer whether to continue or discontinue treatment of such disorders; rather, the issues are which treatments to continue and how they should be administered.
The most important message is that in the ideal case, any woman with a known, preexisting medical condition—neurologic or other—should discuss her plans to become pregnant with her physician before she becomes pregnant.
General Considerations in Women of Childbearing Potential
All women of childbearing potential should be receiving folic acid at a dosage of 0.4 mg/day, in accordance with the recommendation of the US Centers for Disease Control and Prevention (CDC).
If neural tube defects occurred in a woman’s previous pregnancy, increased antepartum fetal surveillance is required for the current pregnancy. This surveillance should include consultation with a geneticist and targeted fetal ultrasonography to assess the fetal spine and cranium. In addition, preconception supplementation with folic acid at 4 mg/day is recommended; this dosage is higher than that advised for a woman without such a history.
Vegetarians, particularly strict vegetarians, need to be aware of the risk of vitamin B-12 deficiency and other vitamin deficiencies. Strong consideration should be given to supplementing vitamin intake and checking levels.
Women planning to become pregnant should avoid all alcohol consumption, smoking, and use of illegal drugs (e.g., cocaine) before and during the pregnancy, because these activities may have serious deleterious effects on the fetus. It is also advisable for the prescribing provider to review all medications and supplements the woman is taking to assess for possible teratogenicity.
All women with neurologic disease who are or wish to become pregnant

Any woman with an existing neurologic condition should consult her obstetrician and her neurologist before she becomes pregnant. During this consultation, the patient can be advised about the possible risks associated with her condition during pregnancy and about the possible teratogenic effects of her medications.
If the woman is already pregnant and did not consult her physician in advance, she must alert her obstetrician and neurologist as soon as possible. Her physicians should review her current medications for their teratogenic potential, and drugs that pose a significant teratogenic risk should be discontinued if possible.
It is important, however, that medications be discontinued only when doing so makes good clinical sense for the mother, not solely because they may be associated with congenital anomalies. For example, if antiseizure medications are stopped prematurely, seizure activity may increase during the pregnancy and eventually expose the fetus to several medications at doses higher than those originally used to control the condition.
At least 2 systems are used to classify the risk associated with specific medications: the US Food and Drug Administration (FDA) system and the automated Teratogen Information System (TERIS). The FDA risk categories are as follows:
- Category A – Controlled human studies show no risk
- Category B – There is no evidence of risk in humans, but no controlled human studies are documented
- Category C – Risk to humans has not been excluded
- Category D – There is positive evidence of risk to humans from human or animal studies
- Category X – Contraindicated in pregnancy
Unfortunately, the correlation between the 2 risk classification systems is poor. According to the TERIS, the teratogenic risk in human pregnancy is undetermined for 91.2% of the drug treatments approved in the United States between 1980 and 2000.
For most drug treatments introduced in the past 2-3 decades, the information available to pregnant women and their physicians is insufficient to determine whether the benefits exceed the teratogenic risks. Therefore, in most cases, the cautionary approach (category C) is based on an absence of information, and individualized discussions between the woman and her treating physicians are required to permit an informed joint decision.
Consider consultation with a physician who has expertise in teratogens (e.g., a geneticist). During this consultation, the possible risks of the patient’s medications can be discussed, as can the risk that the fetus may inherit the condition for which the medications were prescribed.
Breastfeeding women

A classification of the potential effect of medications on breastfeeding infants has been described. This classification is similar to the FDA classification of teratogenicity risk and includes the following categories:
- Contraindicated
- Requires temporary cessation of breastfeeding
- Effect unknown but may be of concern
- Use with caution
- Usually compatible
Like the FDA system, this system tends toward a proscriptive approach when no information is available to confirm that breastfeeding is safe. The absence of information results from the understandable exclusion of pregnant or breastfeeding women or of women who may become pregnant from clinical trials. The result may be overly restrictive.
Again, individualized discussions between the woman and her treating physicians may permit informed joint decision-making, during which the benefits of breastfeeding can be considered and balanced against the potential risks of medications excreted in breast milk.
Medicolegal issues
The following comments regarding medicolegal issues are provided for educational purposes only; they should not be considered all-inclusive, nor should they be construed as legal advice. Clinical practice may vary.
The most obvious medicolegal risks are the following:
- Failure to diagnose a condition that develops during pregnancy
- Failure to preempt teratogenesis or avoid teratogenic medications when possible
- Failure to anticipate and inform or warn the patient about the potential effect of pregnancy on the management or control of preexisting conditions (e.g., epilepsy or sleep apnea)
With regard to magnetic resonance imaging (MRI) during pregnancy in the research setting, in which participation is entirely voluntary and optional, the Johns Hopkins Medicine Internal Review Board has stated that “MRI Imaging is not known to cause risk to the developing fetus though there may be risks that are not known at this time. MRI contrast is known to cross the placenta and subsequent risks to the developing fetus are not known.”
Such language also appears to be adequate in the clinical setting when the indication for the study is clearly articulated and the risk of failure to diagnose is weighed against the unknown and hitherto undemonstrated risk to the developing fetus.
In addition, the risk associated with MRI in a particular clinical situation must be weighed against the risk associated with alternative imaging modalities using ionizing radiation. The chief concern is that an adverse outcome may occur that is unrelated to MRI but will be attributed to imaging. This risk may be minimized by appropriately documenting the indications for the test, discussing the benefits and risks with the patient, and obtaining the patient’s consent to testing.
Similar considerations apply to the clinical use of magnetic resonance angiography (MRA) or magnetic resonance venography (MRV) during pregnancy. The benefits of the information that may be gained from MRA or MRV must be weighed against the understanding that even though no risks are currently documented for these procedures, significant radiation-related risks are documented for alternative testing modalities (e.g., conventional angiography and computed tomographic angiography [CTA]).
New-Onset Neurologic Complications
There are several neurologic complications that occur with some frequency during pregnancy or around the time of delivery in women who were previously free of neurologic disease. Fortunately, serious complications are rare.
Preeclampsia and eclampsia
Eclampsia is defined as the triad of hypertension, proteinuria, and seizures; of these, seizures are the most serious consequence. Preeclampsia is usually diagnosed based on the onset of hypertension and proteinuria in the late second or third trimester.
Preeclampsia can lead to eclampsia. The only known cure for this disease process is delivery. Therefore, when women develop preeclampsia at term, delivery is recommended. However, when preeclampsia occurs at a premature gestational age, attempts may be made to prolong the gestation if it is thought to be in the best interest of the fetus and if the mother’s condition remains stable.
The obstetric conditions usually dictate the mode of delivery. In general, most patients with preeclampsia are treated with magnesium sulfate infusions during labor and for a short time after delivery to prevent eclamptic seizures.
Symptoms usually emerge during gestation. If left untreated, they tend to worsen, with a peak risk at or around the time of delivery. However, the initial presentation may be involved with postpartum seizures in the absence of previously recognized hypertension or current proteinuria.
Patients who have seizures invariably undergo imaging studies to exclude bleeding secondary to hypertension or other structural pathologic conditions. Evidence of reversible posterior leukoencephalopathy (RPLE) (see below) is occasionally seen on imaging studies. Brain images are usually normal.
Treatment of seizures usually includes magnesium sulfate, but benzodiazepines or rapidly acting antiepileptic drugs (AEDs), such as phenytoin, may be required. Generally, long-term AED treatment is not needed once the patient’s blood pressure has returned to normal and stabilized. However, no data are available to determine precisely how long short-term treatment should last; for the most part, local clinical practice prevails.
Reversible posterior leukoencephalopathy
RPLE is also known as reversible posterior leukoencephalopathy syndrome (RPLS) and posterior reversible (leuko-) encephalopathy syndrome (PRES). The 2 most common clinical presentations of RPLE in pregnant women are seizures and postpartum blindness.
RPLE is probably best understood as a condition in which cerebral autoregulation of blood pressure is overwhelmed, usually because of a rapid rise in blood pressure. Vasogenic edema occurs in vulnerable regions. The posterior circulation territory is thought to be most vulnerable because it has a relatively poor ability to autoregulate. Other regions may be involved, and RPLE occasionally affects gray matter.
RPLE is usually identified in settings of hypertensive encephalopathy. Patients with renal failure, those with eclampsia or peripartum seizures, and those taking immunosuppressant or cytotoxic medications are especially susceptible. Metabolic imbalances (e.g., hypomagnesemia) and fluid overload may lower the threshold for precipitation of RPLE by rapidly elevating the patient’s blood pressure.
With appropriate treatment to control blood pressure, clinical and imaging abnormalities usually resolve rapidly. If left untreated, RPLE may progress to permanent infarct or intraparenchymal bleeding.
Cerebral venous thrombosis
In the pregnant patient, cerebral venous thrombosis (CVT) is as common a cause of stroke as cerebral ischemia or cerebral hemorrhage is. CVT is often encountered after delivery. The main symptoms and findings are headache, stroke in a venous distribution, or both. The clinical challenges are as follows:
- To identify CVT in patients presenting with headache alone before it progresses
- To recognize CVT as the correct cause of stroke in a patient presenting in the peripartum period
Without treatment, CVT may lead to the emergence or progression of stroke, exacerbation of dysfunction, worsening of increased intracranial pressure (ICP) that leads to vision impairment, and persistence of a headache that is difficult to treat.
Therapy for CVT consists of anticoagulation with heparin, which after delivery is switched to warfarin. In rare cases, elevated ICP must be treated. However, acetazolamide is a category C drug (meaning that data about risks in humans are not available), and its risks in infants and children have not been studied. Hence, its use must be preceded by a clear definition of goals and by discussions with the patient and her obstetricians. CVT usually, but not always, resolves. Analgesia is permitted, in accordance with usual obstetric practice.
The underlying genetic or acquired risk factors for a hypercoagulable state are often sought. Little is known about the yield of such a search in patients who have no other history of venous thrombosis or of previous fetal loss. However, the presence or absence of risk factors for hypercoagulability may contribute to decision-making about the duration of warfarin therapy. At present, no data are available to guide recommendations about how long the patient should take warfarin.
The question of the optimal duration of warfarin treatment acquires relevance for patients who developed CVT during pregnancy and who wish to become pregnant again, in that warfarin is a category X drug. Reports describe birth malformations in children born to mothers who were treated with warfarin during pregnancy. Furthermore, the drug passes through the placental barrier and may cause fatal hemorrhage in utero.
Consequently, if the decision has been made that the patient requires anticoagulation in her next pregnancy, warfarin should be discontinued, and fractionated or unfractionated heparin should be used instead. All therapeutic decisions must be individualized after discussions with the patient.
Back pain and posterior pelvic pain
A fair number of women have various degrees of back pain or posterior pelvic pain during pregnancy. The 2 conditions are distinguished as follows:
- Back pain refers to nonradiating pain centered in the lower lumbar region
- Posterior pelvic pain refers to pain that is lower and more lateral (buttock); pelvic pain also radiates to the feet in 45-65% of patients (i.e., sciatica)
The presumptive cause of back and pelvic pain is the added mass of a gravid uterus in the context of relaxation of the ligaments supporting the uterus. The 3 treatment options are as follows:
- Adaptive management
- Mechanical support
- Symptomatic therapy
The patient’s activities should be adapted to avoid intolerable pain, and the obstetrician should approve any analgesics.
Compression and stretch neuropathy
Compression or stretch neuropathies occur rarely as postdelivery complications. These conditions are disconcerting to the patient because they introduce unanticipated and unwelcome intrusions into the joyful setting of an expectant family. Dealing with the disappointment of the patient and her family becomes an important focus of therapeutic interventions. The overall prognosis for recovery is excellent, though no immediate guarantee can be given to any individual patient at presentation.
The most common locations at which compression or stretch neuropathies occur are the sciatic nerve (presumably because of positioning during natural delivery) and the femoral nerve (presumably because of retraction during cesarean delivery).
Emergence or worsening of carpal tunnel syndrome may occur during pregnancy. The presumed mechanism is pressure on the median nerve within the carpal compartment at the wrist because of tissue swelling, secondary to the fluid retention that occurs during pregnancy.
The use of spinal or epidural analgesia or anesthesia raises the possibility of a local complication (e.g., bleeding) related to the anesthesia. When adequate localization cannot be achieved by means of the neurologic examination, lumbar spinal magnetic resonance imaging (MRI) may help. MRI may be indicated if the findings suggest a diagnosis or etiology other than compression neuropathy (e.g., a central cause).
A rehabilitation medicine specialist (physiatrist) or physical therapist should be consulted to assist in developing a plan to help the patient ambulate, to choose appropriate assistive devices, and to select appropriate range-of-motion and strengthening exercises for the different stages of recovery. Follow-up with a neurologist, physiatrist, physical therapist, or primary physician must be individualized.
Headache and Migraine

Migraine is extremely common among young women. Hence, optimization of its management during pregnancy is a concern that is relevant to most young female migraineurs. Ideally, management should be optimized before the patient considers pregnancy, and the woman should discuss her plans to become pregnant with the practitioner treating the migraine, so that any medications contraindicated during pregnancy, particularly during early gestation, can be avoided.
Most preventive and mechanism-specific treatments are contraindicated before conception or during pregnancy because the small but definite risk to the fetus cannot be justified in view of the therapeutic alternatives available, even if these alternatives are less effective than the contraindicated drugs.
In December 2009, the US Food and Drug Administration (FDA) posted a statement on its MedWatch Website that highlighted the risks of valproate sodium and related products (valproic acid and divalproex sodium) and encouraged consideration of “alternate therapies, especially if using valproate to treat migraines or other conditions not usually considered to be life-threatening.”
Approximately 60-70% of migraineurs improve spontaneously during pregnancy, usually in the third or fourth month. On occasion, the first migraine attack occurs during pregnancy, usually during the first trimester. New onset of aura may occur during the second and third trimesters.
Headaches often return during the first week postpartum; however, lactation may also affect the presence of headaches. Postpartum headaches occur in about 34% of women, typically from days 3 to 6. Postpartum headache is usually less severe than the typical migraine and is usually bifrontal, prolonged, and associated with photophobia, nausea, and anorexia.
The onset of a new severe headache, especially in a nonmigraineur, should prompt evaluation of other diagnoses (e.g., intracranial hemorrhage, temporal arteritis, internal carotid dissection, cerebral venous thrombosis [CVT], reversible posterior leukoencephalopathy [RPLE], meningitis, and pituitary apoplexy). New onset of migraine with aura can be caused by vasculitis, brain tumors, and occipital arteriovenous malformations.
Some brain tumors grow rapidly during pregnancy (e.g., including meningiomas, choriocarcinomas, and pituitary tumors. Arteriovenous malformations have been found more commonly during pregnancy and tend to bleed in the middle toward the end of pregnancy; aneurysms are more likely to bleed during weeks 30-40. CVT occurs most frequently in the peripartum period.
Several retrospective studies showed that migraineurs are not at increased risk of miscarriage, toxemia, congenital malformations, and still births. A subsequent prospective study found that relative to 3.1% of nonmigraineurs, 9% of migraineurs had hypertensive disorders during pregnancy. There was also a trend toward a higher rate of low-birth-weight infants in the migraine group.
Pharmacologic options for the treatment of headaches during pregnancy (see Table 1 below) are limited and should be avoided if possible. Acceptable agents for acute attacks include acetaminophen, caffeine, and opioids. Ibuprofen and naproxen are also acceptable before the third trimester. Caffeine is particularly effective for women who do not habitually consume caffeine and women in whom caffeine withdrawal does not trigger migraine. Antiemetics that may be considered for use during pregnancy are prochlorperazine and promethazine.
Table 1. Pregnancy and Breastfeeding Risk for Medications Used to Treat Migraine.
| Generic Name | Level of Risk in Pregnancy | Breastfeeding |
| Acetaminophen | B | Caution |
| Dihydroergotamine | X | Contraindicated |
| Ergotamine | X | Contraindicated |
| 5-HT1 agonists | C | Probably compatible |
| Aspirin | C (D in 3rd trimester) | Compatible |
| Caffeine | B | Compatible |
| Ibuprofen | B (D in 3rd trimester) | Compatible |
| Naproxen | B (D in 3rd trimester) | Compatible |
| Codeine | C (D at term or prolonged use) | Compatible |
| Meperidine | B (D at term or prolonged use) | Compatible |
| Morphine | B (D at term or prolonged use) | Compatible |
| Prednisolone | C (D in 3rd trimester) | Compatible |
| Prochlorperazine | C | Concern |
| 5-HT1 = serotonin receptor subtype 1. |
Treatment options for a severe acute attack (status migrainosus) include intravenous hydration, antiemetics, analgesics, and steroids.
Ergotamines are contraindicated (risk category X), and triptans are not recommended (risk category C; risk cannot be ruled out), but as of 2011, the sumatriptan and naratriptan registry had not found an increased risk of first-trimester birth defects.
In addition, various medications may be used to prevent migraines, and these are also associated with varying levels of pregnancy and breastfeeding risk (see Table 2 below).
Table 2. Pregnancy and Breastfeeding Risk for Medications Used to Prevent Migraine
| Drug Class | Generic Name | Level of Risk in Pregnancy | Breastfeeding |
| Beta blockers | Atenolol | D | Caution |
| Metoprolol | C (D at term or prolonged use) | Compatible | |
| Nadolol | C (D at term or prolonged use) | Compatible | |
| Propranolol | C (D at term or prolonged use) | Compatible | |
| Timolol | C (D at term or prolonged use) | Compatible | |
| Antiepileptics | Gabapentin | C | Probably compatible |
| Topiramate | C | Caution | |
| Valproate | D | Compatible | |
| Calcium channel blocker | Verapamil | C | Compatible |
| Tricyclics | Amitriptyline | C | Concern |
| Imipramine | C | Concern | |
| Nortriptyline | C | Concern | |
| Serotonin antagonist | Methysergide | D | Contraindicated |
Epilepsy
Most women of childbearing potential who have epilepsy expect to become pregnant. Epilepsy is not in itself a contraindication to pregnancy; however, seizure management should be optimized before pregnancy is considered. If seizures are not acceptably controlled, attention to compliance is recommended. Furthermore, video, or electroencephalographic (EEG) monitoring is recommended for classifying intractable seizures before conception to optimize treatment and minimize the risk to the woman and the fetus.
Patients with mixed (i.e., epileptic and nonepileptic) seizure types who are noncompliant with pharmacotherapy pose a particularly challenging management situation.
A fair amount of information is available on how to optimize seizure management while minimizing maternal and fetal risk. Preconception discussions between the woman and her health care provider and consultation with a neurologist provide the best opportunities for applying this information to a particular pregnancy.
Three practice parameters published in 2009 by the American Academy of Neurology (AAN) and the American Epilepsy Society (AES) provide valuable information for women with epilepsy who are pregnant or planning to become pregnant. The AAN/AES guidelines affirm that in general, it is safe for women with epilepsy to become pregnant, but they make specific suggestions with regard to managing the medications these women are taking before and during pregnancy (see below).
Folic acid supplementation
The AAN/AES guidelines state that preconception folic acid supplementation is possibly effective in preventing major congenital malformations in the newborns of women with epilepsy taking antiepileptic drugs (AEDs). This is a Centers for Disease Control and Prevention (CDC) recommendation for all women of childbearing potential. The optimal dose for women with epilepsy has not been determined, and the guidelines suggest that giving these women at least 0.4 mg/day of folic acid before they become pregnant may be considered.
The authors’ practice is to provide folic acid supplementation at a dosage of 4 mg/day to women taking AEDs who are planning to become pregnant. One report found that folic acid supplementation was associated with a significant reduction in spontaneous abortion. Among women on monotherapy, this effect was evident for those taking valproate but not those taking carbamazepine, phenytoin, or phenobarbital, possibly because of the reduced baseline teratogenicity of the last 3 drugs relative to that of valproate.
Antiepileptic drugs in pregnancy
The AAN/AES guidelines state that there probably is no substantially increased (> 2 times expected) risk of cesarean delivery or late pregnancy bleeding, and no moderately increased (> 1.5 times expected) risk of premature contractions or premature labor and delivery in pregnant women taking AEDs. However, for women with epilepsy who smoke, there may be a substantially increased risk of premature contractions and premature labor and delivery during pregnancy.
In addition, the guidelines state that women with epilepsy who are seizure-free for at least 9 months before pregnancy probably have a high likelihood (84-92%) of remaining seizure-free during pregnancy.
Monitoring of AED levels
The AAN/AES guidelines state that pregnancy probably increases the clearance and decreases the concentration of lamotrigine, phenytoin, and, to a lesser extent, carbamazepine and that it possibly decreases the level of levetiracetam and the active oxcarbazepine metabolite, the monohydroxy derivative. They state that monitoring of lamotrigine, carbamazepine, and phenytoin levels during pregnancy should be considered and suggest that monitoring of levetiracetam and oxcarbazepine levels may be considered.
Mild, nonspecific effects of AEDs on fetus
The AAN/AES guidelines state that the neonates of women with epilepsy who are taking AEDs probably have an increased risk of being small for gestational age (SGA) and possibly have an increased risk of a 1-minute Apgar score lower than 7.
Risks of antiepileptic drug polytherapy for fetus
In general, monotherapy is preferable to polytherapy when AEDs are used, and this is particularly true during pregnancy. The risk of major malformations is as high as 25% in infants of women who are taking 4 or more AEDs. The AAN/AES guidelines state that AED polytherapy, as compared with monotherapy regimens, probably contributes to the development of major congenital malformations and to reduced cognitive outcomes in the fetus, and they recommend avoidance of polytherapy if possible.
Risks of valproate therapy for fetus
According to the AAN/AES guidelines, it is highly probable that intrauterine first-trimester valproate exposure carries a higher risk of major congenital malformations than carbamazepine exposure, and it is possible that it carries a higher risk than phenytoin or lamotrigine exposure. Valproate as part of polytherapy probably contributes to the development of major congenital malformations, and valproate as monotherapy possibly contributes. For monotherapy, intrauterine exposure to valproate probably reduces cognitive outcomes.
Meador et al reported that in utero exposure to valproate, compared with exposure to other AEDs, is associated with a lower intelligent quotient (IQ) in children. This report derived from a prospective, observational, cohort study of pregnant women with epilepsy who took a single agent (carbamazepine, lamotrigine, phenytoin, or valproate) over a period of 5 years in 25 epilepsy centers in the United States and the United Kingdom.
The cohort study assessed the neurodevelopmental outcomes of children who were exposed in utero to several AEDs. A planned interim analysis conducted when the children were aged 3 years found an increased risk of impaired cognitive function with valproate as compared with other commonly used antiepileptic drugs and determined that this association was dose dependent. The investigators concluded that valproate should not be used as a first-line agent in women of childbearing potential.
A report based on analysis of data from the Neurodevelopmental Effects of Antiepileptic Medications (NEAD) study (Baker GA, World Congress of Neurology, 2009), indicated that the receptive and expressive language abilities of 3-year-olds who were exposed to sodium valproate in utero were lower than those of children who had been exposed to other AEDs.
In this report, the average score on measures of an expressive language for 3-year-olds exposed to valproate in utero was 91, compared with 102 for those exposed to carbamazepine, 104 for those exposed to lamotrigine, and 101 for those exposed to phenytoin. On measures of receptive language, the average score for children exposed to valproate in utero was 89, compared with 97 for those exposed to carbamazepine and 101 for those exposed to lamotrigine or phenytoin.
A 2015 study from the United Kingdom extends these observations to school-aged children. It reports on outcomes of children born to women with epilepsy (n=243) and women without epilepsy (n=287) who were recruited during pregnancy and followed prospectively. Of the total cohort of children, 408 were blindly assessed at 6 years of age. Consistent with data from younger cohorts, school-aged children exposed in utero to valproate at maternal doses more than 800 mg daily continue to experience significantly poorer cognitive development than control children or children exposed to lamotrigine and carbamazepine.
The adjusted mean IQ was 9.7 points lower for children exposed to high-dose (>800 mg daily) valproate, with a similar significant effect observed for the verbal, nonverbal, and spatial subscales. These children also had an 8-fold increased need of educational intervention relative to control children. Valproate at doses < 800 mg daily was not associated with reduced IQ, but was associated with impaired verbal abilities (−5.6, 95% CI −11.1 to −0.1; p = 0.04) and a 6-fold increase in an educational intervention (95% CI 1.4–18.0; p = 0.01). In utero exposure to carbamazepine or lamotrigine did not have a significant effect on IQ, but carbamazepine was associated with reduced verbal abilities (−4.2, 95% CI −0.6 to −7.8; p = 0.02) and increased frequency of IQ < 85.
Risks of carbamazepine, nonvalproate AED, phenytoin, and phenobarbital monotherapy for fetus
A review of all published cohort studies yielded an overall prevalence of 3.3% for a major congenital malformation after exposure to carbamazepine monotherapy during the first trimester of pregnancy.
Spina bifida was the only major congenital malformation associated with carbamazepine as compared with no AED. The risk was smaller with carbamazepine than with valproate. However, the risk of spina bifida with carbamazepine was no different from that with other nonvalproate AEDs.
The risk of fetal hypospadias with mothers taking carbamazepine was comparable to that with mothers taking other nonvalproate AEDs and lower than that with mothers taking valproate. The risk of cleft lip, with or without cleft palate, was lower for carbamazepine monotherapy than for other nonvalproate AED monotherapy (phenobarbital in more than 50% of cases) or for valproate (though the difference in this case, was statistically nonsignificant).
Overall, therefore, the risks of carbamazepine to the fetus are smaller than those of valproate and comparable to those of other nonvalproate AEDs, except for the lower risk of cleft lip, with or without cleft palate, on carbamazepine.
The AAN/AES guidelines state that exposure to phenytoin or phenobarbital monotherapy possibly reduces cognitive outcomes.
Risks of lamotrigine therapy for fetus
The North American Antiepileptic Drug (NAAED) pregnancy registry reported an elevated prevalence of isolated, nonsyndromic oral clefts in infants exposed to lamotrigine monotherapy during the first trimester as compared with a reference population.
A “Dear Health Professional” letter issued by the manufacturer reported 5 cases of oral clefts among 564 pregnancies exposed to lamotrigine during the first trimester, for a rate of 8.9 cases per 1000 pregnancies. The letter stated that this rate is 24 times higher than the prevalence of 0.37 cases per 1000 pregnancies in the general population of the surveillance program of Brigham and Women’s Hospital.
An FDA alert in September 2006, Information for Healthcare Professionals: Lamotrigine (marketed as Lamictal), (accessed March 30, 2011) stated the following:
“Preliminary data from the North American Antiepileptic Drug Pregnancy Registry suggest a possible association between exposure to lamotrigine monotherapy during the first trimester of pregnancy and cleft lip and/or cleft palate. The oral clefts reported were few and were not part of a syndrome that included other birth defects. Other pregnancy registries of similar size have not replicated this observation. The validity of this possible association cannot be established until further data are collected in the NAAED Pregnancy Registry, in other ongoing pregnancy registries, or through other research efforts. The clinical significance of this preliminary report is thus uncertain.”
The differences among the different series may be related to the levels of lamotrigine attained in the sera of the mothers and fetuses; presumably, teratogenicity is less with lower levels, but data confirming this hypothesis are lacking.
Frequencies of adverse events with specific agents
Data are available from the NAAED pregnancy registry about major malformations associated with monotherapy. The rates for AEDs are as follows:
- Phenobarbital (n = 77) – 6.5%
- Valproic acid (n = 143) – 10.7%
- Other AED (n = 1048) – 2.9%
- No AED (active malformation surveillance program) – 1.62%
Data from the Lamotrigine Pregnancy Registry showed rates of 2% with monotherapy and 12.1% for lamotrigine plus valproic acid. One study reported a rate of fetal death or major congenital malformations of 20% for valproic acid, 11% for phenytoin, 8% for carbamazepine, and 1% for lamotrigine.
Bleeding risk
The AAN/AES guidelines state that the evidence is insufficient to determine whether the newborns of women with epilepsy who are taking AEDs have a substantially increased risk of hemorrhagic complications. Anecdotal evidence suggests an increased risk of bleeding in mothers taking AEDs and in newborns because of the potential for vitamin K deficiency arising from the increased vitamin K metabolism induced by some AEDs.
A possible remedy for the deficiency is for the mother to take vitamin K 10 mg orally during the last month of pregnancy; as an alternative, vitamin K may be given parenterally during labor. The newborn should receive 1 mg either intramuscularly (IM) or intravenously (IV) at birth. However, these recommendations are not followed universally, because the evidence to support them is anecdotal.
Breastfeeding on AED therapy
The AAN/AES guidelines state that primidone and levetiracetam probably transfer into breast milk in amounts that may be clinically important; valproate, phenobarbital, phenytoin, and carbamazepine probably are not transferred into breast milk in clinically important amounts. In addition to this general classification, the following information may be useful for decision-making regarding breastfeeding by women taking AEDs to treat epilepsy.
Breast milk–maternal plasma ratios for AED concentrations are as follows:
- Carbamazepine – 0.4
- Phenytoin – 0.45
- Phenobarbital – 0.4-0.6
- Valproic acid – 0.42
- Lamotrigine – 0.6
If carbamazepine is maintained at a serum level of 8 µg/mL, the breast milk–serum concentration ratio is 0.4, and the newborn’s daily milk intake is 200 mL, then the daily intake of carbamazepine is 640 µg/day, or 0.64 mg/day. Thus, for a 3.5-kg newborn, intake is about 0.2 mg/kg/day. However, the newborn’s metabolism of carbamazepine is less efficient than the mother’s, prolonging the drug’s half-life. This prolongation yields an intake equivalent to 1 mg/kg/day in a person with normal clearance, which appears to be a negligible intake.
Similar calculations may be performed for the other AEDs. However, results may be less favorable for medications with long half-lives, such as phenobarbital, lamotrigine, and valproate combined, or concomitant non-AED medications associated with impaired metabolism in newborns.
One report reported undetectable levels of antidepressants and benzodiazepines in the sera of breastfed infants of mothers who were taking these medications only during lactation. The number of mother-infant pairs was limited; however, the results may be dose-related and thus may not be generalizable to mothers taking higher doses of these medications.
Therefore, the potential risks associated with breastfeeding by a mother taking AEDs may have to be considered on a case-by-case basis. In some patients, particularly those on monotherapy, the risks may be related less to serum levels than to idiosyncratic reactions. However, because the newborn is exposed to medications in utero, opportunities for idiosyncratic reactions to occur are ample even before birth and therefore need not be overstated after birth.
Moreover, abrupt discontinuance of AEDs may pose some risks to newborns who were exposed to them in utero; effects include jitteriness (a withdrawal symptom) and, in rare cases, seizures. Withdrawal symptoms are most common with benzodiazepines.
If a decision is made to refrain from breastfeeding while on AEDs, some practitioners recommend initial breastfeeding for 2 weeks, with progressive discontinuance over another 2 weeks. Because the baby had been exposed for the preceding 9 months, the gradual downward titration of AED levels in the infant might potentially minimize withdrawal symptoms.
The official labeling of most, if not all, AEDs recommends that breastfeeding women not use these agents. However, this recommendation appears to be an oversimplification of the situation because the benefits of breast milk to the infant may outweigh the risks of low levels of AEDs.
Results from the Neurodevelopmental Effects of Antiepileptic Drugs Study, which included 199 children who had been exposed to a single AED (carbamazepine, lamotrigine, phenytoin, or valproate) in utero, showed no overall intelligence quotient (IQ) differences at age 3 years between those who subsequently were breastfed and those who were not.
The results for phenytoin trended in the opposite direction from those for the other AEDs, but the 95% confidence intervals for the 2 groups overlapped. Nevertheless, the general conclusion may not apply to phenytoin. Women taking phenytoin may need to be advised differently about the safety of breastfeeding. The study affirmed the finding that children exposed in utero to valproate had a lower IQ at age 3 years.
Ideally, therefore, a mother’s choice regarding breastfeeding and concomitant use of AEDs should be guided by an informed, patient-specific decision process.
Specific treatment recommendations
Specific treatment recommendations for epilepsy in pregnant women should be individualized. The risk to the fetus should be balanced with the risk to the woman posed by generalized tonic-clonic seizures or, if the woman is seizure-free before conception, by breakthrough seizures of any type during pregnancy.
The authors’ standard practice is to try to achieve monotherapy before pregnancy, if possible, by aiming for the best medication for the specific seizure type. Valproic acid and phenobarbital are avoided if possible. Concomitant nonepileptic medications are reviewed, and those that can be eliminated should be discontinued.
The authors also recommend supplementation with folic acid at a dose of 4 mg/day, while conceding that no evidence supports the use of this dosage rather than a lower dosage, such as 0.4 mg/day.
In addition, increased fetal surveillance is recommended if the woman requires treatment with AEDs. This surveillance should include a detailed anatomic survey with high-resolution ultrasonography, fetal echocardiography, and maternal serum screening for alpha-fetoprotein, which assists in diagnosing neural tube defects.
The authors prefer to check AED levels frequently (e.g., monthly) because levels may drop during pregnancy and rise after delivery. The dosage is adjusted if necessary.
Pregnant women taking antiepileptic medications should be encouraged to enroll in the NAAED Pregnancy Registry online or at 888-233-2334.
Sleep Disorders

Symptoms related to sleep (e.g., insomnia, sleep apnea, hypersomnia, and parasomnias) are more common in pregnant women than in nonpregnant women. Pregnant women are most likely to snore and to have insomnia and daytime sleepiness. A variety of factors may contribute to this increase in symptoms, including weight gain, hormonal changes, nutritional stress, and nocturnal discomfort.
Insomnia
Insomnia is most prevalent in the first and third trimesters and affects a substantial minority of pregnant women. Causes include urinary frequency, low back pain, nocturnal cramps, fetal movements, and restless legs syndrome (RLS) or periodic limb movements of sleep.
Urinary frequency often occurs early in pregnancy and may result in repeated bouts of nocturia.
Low back pain is a common symptom among pregnant women. The weight of the enlarging uterus stresses the spine and changes lumbar posture. The sleeping position may have to be changed to one that minimizes backache. Specially shaped pillows have been recommended and offer some benefit. Water exercises, physical therapy, and acupuncture may also reduce discomfort, improve function, and lessen insomnia.
Nocturnal cramps occur more frequently during pregnancy than in other stages of life. The cause of these painful, sleep-disrupting attacks usually cannot be determined. Several trials of vitamin and mineral supplements have been published, but little benefit from such treatments is documented. The available data give the greatest support to the use of magnesium salts to decrease cramps.
Fetal movements become increasingly prominent as the pregnancy progresses, and they may contribute to nocturnal arousals in certain patients.
RLS may occur throughout life but is unusually prevalent during pregnancy. In this disorder, the patient reports a distinctly unpleasant, nearly continuous urge to move her legs late in the day and at night. The symptoms can be a major obstacle to falling asleep. Once asleep, a patient may have periodic leg movements that can cause several arousals.
Data from epidemiologic and other investigations support the notion that iron deficiency may play a role in the genesis of RLS. Iron is a cofactor in the endogenous production of dopamine in the central nervous system (CNS). Dopamine, in turn, plays a role in modulating movement. The altered dopaminergic balance can result in restlessness. This is seen in association with Parkinson disease and in the akathisia that may accompany the use of neuroleptic drugs, which are known to block dopamine receptors.
Folate is another nutrient that may play a role in the prevention of RLS. In a group of pregnant women, those with low serum folate levels were most likely to have restless legs.
Dopamine receptor agonists have been highly effective in relieving RLS, but their safety during pregnancy has not been demonstrated; other proven treatments include narcotics, benzodiazepines, certain antiepileptic drugs (AEDs), and clonidine. These agents are associated with varying levels of risk to the fetus (see Table 3 below).
Table 3. Risks of Drug Therapies for Restless Leg Syndrome in Pregnancy
| Drug Class | Generic Name | Level of Risk in Pregnancy |
| Dopaminergic | Carbidopa-levodopa | C |
| Bromocriptine | B | |
| Pergolide (removed from US market March 29, 2007*) | B | |
| Pramipexole | C | |
| Ropinirole | C | |
| Opioid | Oxycodone | B |
| Propoxyphene | C (D for long-term use) | |
| Tramadol | C | |
| Benzodiazepine | Clonazepam | D |
| Diazepam | D | |
| Lorazepam | D | |
| Antiepileptic | Gabapentin | C |
| Carbamazepine | D | |
| Alpha-agonist | Clonidine | C |
* Pergolide was withdrawn from the US market on March 29, 2007, because of heart valve damage resulting in cardiac valve regurgitation. It is important not to stop pergolide abruptly. Healthcare professionals should assess patients’ need for dopamine agonist therapy and consider alternative treatment. If continued treatment with a dopamine agonist is needed, another dopamine agonist should be substituted for pergolide.
Because RLS has a benign prognosis and often resolves after pregnancy, most women are reluctant to receive pharmacologic treatment. Increased supplementation of iron and folate may be the best approach. In addition, because the serum ferritin level may not directly reflect the availability of iron in the CNS, iron supplementation to achieve a ferritin level above the minimal normal level should be considered. Additional folate intake beyond the recommended daily allowance of 400 µg may also be warranted.
Sleep apnea
Although elderly men have the risk of obstructive sleep apnea, sleep-disordered breathing may also occur in pregnant women. The prevalence of loud snoring is reported to increase during the late months of pregnancy. Women who gain excessive weight or develop fluid retention may be at particular risk for reduced airflow (i.e., apneic and hypopneic events). Such irregularities in breathing degrade the quality of nighttime sleep and may lead to daytime sleepiness.
Possible nocturnal oxygen desaturation is another issue for pregnant women, especially during rapid eye movement (REM) sleep. REM sleep typically produces a generalized loss of muscle tone (except in the diaphragm). Consequently, patients with restrictive lung disease may breathe at abnormally low lung volumes during REM sleep. When lung volumes are low, blood may be shunted through underventilated lung tissue, and oxygen desaturation may result. The abdominal distention caused by a gravid uterus may produce or add to a preexisting restriction.
Sleep apnea is a recognized risk factor for hypertension. It may cause recurrent activation of the sympathetic nervous system in response to airway obstruction and hypoxemia. Women with preeclampsia are most likely to have narrow upper airways and to be snorers; this observation suggests that increased upper airway resistance or the resultant snoring or apneas may contribute to pregnancy-induced hypertension. More sleep-disordered breathing is seen in preeclamptic women than in nonpreeclamptic women.
Pregnant women who have an elevated apnea-hypopnea index can be successfully treated with nasal continuous positive airway pressure (NCPAP) therapy, and their blood pressure can be decreased.
Hypersomnia
Daytime sleepiness is another common symptom during pregnancy, but its severity and effect on well-being have not been thoroughly studied. Hormonal changes are suspected to be a contributing factor in the first trimester. After this period, disrupted nighttime sleep may be a substantial factor. Sleep apnea may be the cause in an obese woman who snores.
Particularly in the presence of hypertension, nocturnal polysomnography (multichannel sleep study) may be warranted to diagnose the disorder. NCPAP therapy may be started if indicated, depending on the severity of the condition.
Patients with previously diagnosed narcolepsy or idiopathic CNS hypersomnia may become pregnant and require changes in their treatment. Commonly used stimulants have not been shown to be safe in pregnancy, and these agents should be withdrawn from most patients before conception. An inability to drive safely and an overall decline in functional status may result. For the stimulants dextroamphetamine, methylphenidate, and modafinil, the level of risk to the fetus is category C.
Since 2002, sodium oxybate (gamma-hydroxybutyrate; GHB) has been available to treat narcolepsy. It is a highly sedating compound that is known as a drug of abuse. Sodium oxybate is taken only at night and reduces both cataplexy and daytime sleepiness through unknown mechanisms. The absence of teratogenicity in animal studies has led to it being classified as category B.
Thus, sodium oxybate might be preferable to stimulants during pregnancy, but whether this is so has not been established in clinical trials. Because of its potential for respiratory suppression, sodium oxybate could be harmful to pregnant women with sleep apnea, hypoxemia, or hypoventilation. The maximum recommended dosage is a daily sodium load of 1.6 g, which may be undesirable in pregnant women with edema or hypertension.
Parasomnias
Sleep walking, night terrors, and other parasomnias may occur in women of childbearing age. A few systematic studies have been conducted to investigate the effect of pregnancy on these disorders. Data on whether symptoms may increase or decrease during pregnancy are conflicting. Because benzodiazepines are often given to treat parasomnias and because they may be harmful to the fetus, an attempt should be made to withdraw these agents before conception or, in unplanned pregnancies, early in the first trimester.
Effects of Multiple Sclerosis on Pregnancy
Complications of pregnancy are generally thought to affect women with multiple sclerosis (MS) no more often than they affect women in the general population. This belief extends as far back as 1948 and is supported by data from numerous subsequent studies of fertility, pregnancy, and delivery. Data also suggest that the risk of spontaneous abortions, congenital malformations, stillbirths, and complications of pregnancy (e.g., preeclampsia, premature delivery) is not increased.
Although many findings weigh against the idea that there is a higher risk of low birth weight in infants of mothers with MS, a retrospective study of the Norwegian national registry showed an increased rate of neonates being small for their gestational age (SGA). These neonates had a reduced mean birth weight and length but normal head circumference. The etiology was unclear, though the subtle morphologic changes in the pelvic organs of women with MS may result in suboptimal intrauterine conditions that influence fetal development.
The data also suggested an effect on deliveries. Although the number of planned cesarean deliveries increased, women delivering vaginally had an increased incidence of slow labor progression necessitating interventions. This result may have been partly due to perineal weakness and spasticity and fatigue related to MS.
These findings were countered by those of a 3-year prospective study that reported normal distributions of weight and head circumferences in babies born to mothers with multiple sclerosis. Rates of infant death, congenital anomalies, and cesarean deliveries were also like those of the general population.
The reasons for the discrepancies in these studies are unclear. It is certainly possible that differences in the severity and localization of disease in the patient populations of each study could play a role in the outcomes, particularly if perineal and bladder involvement differed. Factors increasing the frequencies of pelvic infections may also play a role.
Although MS is unlikely to have a serious effect on pregnancy, each patient should be evaluated on an individual basis. Patients with clinically significant bladder and perineal involvement and excessive fatigue should be counseled about possible interventions that may help facilitate delivery.
Effects of pregnancy on multiple sclerosis
An Israeli study of 338 women conducted to evaluate the MS relapse rate during each trimester of pregnancy and 6 months after delivery reported that of 199 completed pregnancies in 66 women, 85 were accompanied by relapses (20 during pregnancy, 65 postpartum). The relapse rate was reduced in the third trimester.
In a later study, Salemi et al reported a significant reduction in the relapse rate during pregnancy. Using a questionnaire, the investigators collected information concerning patient age at the onset of MS, duration of disease, number of relapses during the prepregnancy period, number of relapses during pregnancy, and number of relapses during the first 3 months after delivery. Out of 350 patients, 70 had 98 pregnancies.
The Pregnancy in Multiple Sclerosis (PRIMS) study was the first multicenter prospective study of MS in pregnant women. In this study, the relapse rate declined by approximately 70% during the third trimester as compared with the rate in the year before conception. The researchers evaluated 254 women with relapsing-remitting MS during and after 269 pregnancies. Patients were examined at 20, 28, and 36 weeks’ gestation to determine the relapse rate in each trimester.
Roullet et al reported that MS relapses occurring during pregnancy tended to be mild, resulting in minimal or no residual deficits. They examined the severity of relapses in 125 French women who were followed via an MS clinic over 10 years and who had a total of 32 full-term pregnancies.
Patients with MS appear to fare better when they are pregnant (particularly in the third trimester) than when they are not, with a decrease in the number and severity of relapses. Some authors claim that the suppression of MS seen during pregnancy may be more potent than that achieved with currently available treatments.
Nevertheless, the decision whether to forgo treatment with immunomodulatory agents must be made on an individual basis. Given the potential risks these treatments pose for pregnant women, the decision to treat should be reserved only for exceptional cases (see Treatments during pregnancy).
Postpartum period
In the first 3 months after delivery, MS relapses appear to increase in frequency and severity, though they return to their prepregnancy level afterward. Because this increase is offset by the decrease in MS activity during pregnancy, pregnancy does not seem to change the overall course of the disease from the perspective of disability.
Patients with the relatively severe disease before and during pregnancy appear to be at greatest risk for relapses in the postpartum period. No other single predictor was identified. In these patients, therapies that may reduce the likelihood of relapses should be considered.
In an early study, Millar et al evaluated 45 pregnancy-associated relapses in 170 pregnancies and reported that 39 women experienced relapses in the postpartum period.
Worthington et al observed that relapses were most frequent during the first 6 months after pregnancy and that fewer relapses than expected occurred in postpartum months 6-24. The investigators conducted a 3-year prospective study of the level of disability, severity, and distribution of relapses in 15 women with MS diagnosed before pregnancy, using 22 nulliparous women with the disease as control subjects.
Salemi et al retrospectively determined that the relapse rate increased in the first 3 months after delivery, though the change was not statistically significant.
In a study of 338 women, Korn-Lubetzki et al found that postpartum exacerbations of MS were 3 times more common in patients than in control subjects.
In the Pregnancy in Multiple Sclerosis (PRIMS) study, the postpartum relapse rate increased by approximately 70% and then returned to the pre-pregnancy rate. Neither breastfeeding nor epidural analgesia affected the rate of relapse or progression of disability.
In a study of 227 women enrolled in the PRIMS study for an additional 2 years after delivery, Vukusic et al reported that women with increased disease activity in the year before pregnancy and those who had additional relapses during pregnancy were most likely to have postpartum relapses. The investigators did not find a single predictor (including breastfeeding or epidural anesthesia) that helped in accurately identifying women with MS who would have relapses in the first 3 months after delivery.
In the second postpartum year, the relapse rate was like that of the year before pregnancy. In addition, pregnancy, delivery, and the postpartum period did not ultimately increase overall disability from MS.
Roullet et al also found that relapses were most severe during the postpartum period, as reflected by a change of more than 1 point in the Expanded Disability Status Scale (EDSS) score. Worthington et al confirmed this result, finding that relapses were most severe during the first 6 months after pregnancy.No overall significant differences in the severity of relapses were found between patients and control subjects, as measured by using the median EDSS score after the pregnant and postpartum periods.
Epidural anesthesia did not appear to affect the rate of relapse or progression of disability in either the PRIMS trial or its 2-year extension. This finding suggests that despite anecdotal reports suggesting otherwise, epidural analgesia is safe and does not carry a significant risk when it is used for deliveries in patients with MS.
Breastfeeding
Breastfeeding does not appear to have a notable effect on the activity of MS. However, it does lower the incidences of infantile illnesses, which suggests that it confers some protection on the infant. This finding potentially supports the consideration of breastfeeding and the delay of immunomodulating therapy until breastfeeding is stopped in patients with MS. These potential benefits should be weighed against the risks of delaying treatment on a case-by-case basis.
In a questionnaire-based retrospective study that evaluated the onset of MS, relapse frequency, and breastfeeding in 438 women, half of the patients breastfed their children for a mean of 6.3 months, but the relapse rate in the breastfeeding group was not significantly different from that in the control subjects.
In addition, the mean time to relapse was not delayed with breastfeeding; in fact, 69% of relapses in the breastfeeding group occurred while the patient was still breastfeeding. The study data suggested that breastfeeding did not extend the protective effects of pregnancy on exacerbations of MS.
Indeed, Vukusic et al reported that women who chose to breastfeed had fewer relapses than other women did. However, the investigators also found that the women who chose to breastfeed had relatively mild disease. Conversely, women with active disease (and additional relapses) chose not to breastfeed.
In a study that assessed the incidence of various infantile illnesses at age 6, 9, and 12 months in the children of 140 breastfeeding mothers and 35 nonbreastfeeding mothers, the infants who were not breastfed had significantly higher incidences of otitis media, lower respiratory tract illnesses, constipation, milk intolerance, and allergies.
Treatments during pregnancy

How best to treat pregnant women with MS remains controversial? Although some claim that the suppression of MS during pregnancy is more potent than that achieved with currently available therapies for the disease, it is not clear whether this claim holds true in all cases.
Interferons (category C)
Although interferon beta-1a (IFN-β1a) and interferon beta-1b (IFN-β1b) are category C agents, sufficient data are available from published reports to indicate that they should not be used in pregnant patients, because they impose a high frequency of serious risks on the fetus.
In a rhesus monkey model, high doses of IFN-β1a were not teratogenic but had a dose-dependent abortive effect. In a longitudinal, 3-pronged cohort study involving a group exposed to IFN-β1a and IFN-β1b, a disease-matched unexposed group, and a healthy control group, mean birth weight decreased and rates of miscarriages and stillbirths increased in the exposed group as compared with the control group (39.1% vs 5%). Two major malformations were also identified: An X chromosomal abnormality and Down syndrome.
In another study, 41 pregnancies involving IFN-β1a exposure resulted in 20 healthy full-term infants, 1 healthy premature infant, 9 induced abortions, 8 spontaneous abortions, and 1 fetal death; 1 patient had hydrocephalus, and another was lost to follow-up. These findings were in stark contrast to those of the 22 control subjects, who were exposed to IFN-β1a before, but not during, pregnancy. This control group included 20 full-term healthy infants, 1 healthy premature infant, and 1 infant with a birth-related complication (Erb palsy).
Glatiramer acetate (category B)
An abstract presented at a meeting of the American Academy of Neurology (AAN) in 2003 suggested that glatiramer acetate imposes no substantial risks in pregnancy and has no abortifacient or teratogenic effects. This drug is not known to be excreted in breast milk. Evidence suggests that glatiramer acetate might be safe in pregnancy and breastfeeding. However, caution should be exercised if one decides to treat patients with this drug.
Mitoxantrone (category D)
Mitoxantrone has been associated with low birth weight and abnormal fetal kidney development in animal studies. Rats treated with mitoxantrone had an increased incidence of preterm labor. Because of its known risk in pregnancy, mitoxantrone should not be used in pregnant patients.
Intravenous immunoglobulin (category C)
Orvieto et al suggested that intravenous immunoglobulin (IVIg) has no known teratogenic effects. It also appears to have no effects on the immune system of the fetus or newborn. If necessary, treatment with IVIg may be considered, though the potential risks must be carefully assessed.
Azathioprine (category D)
Despite azathioprine’s category D rating, some believe that this agent is potentially useful for treating MS in pregnancy. Although azathioprine crosses the placenta, the fetus lacks the enzymes that convert the drug into its active metabolites; this lack may protect the fetus from the potential teratogenic effects of azathioprine. Nevertheless, given the category D rating, the use of this drug in pregnancy should be avoided if at all possible.
Methotrexate (category X)
Methotrexate is known to be capable of causing malformations and abortifacient effects. It has a category X rating and should not be used in pregnant patients.
Cyclophosphamide (category D)
Cyclophosphamide is teratogenic in animals, but whether it is also teratogenic in humans has not been clearly determined. Nevertheless, it is a category D agent and therefore should be avoided in pregnant patients.
Corticosteroids (methylprednisolone) (category C)
The PRIMS study included 16 pregnant women who received corticosteroids; no adverse effects were noted in either the patients or their children. Corticosteroids (e.g., methylprednisolone) may be safe in pregnancy. However, use of these drugs in pregnant patients should be considered carefully and avoided unless deemed necessary.
Possible postpartum treatments
There is some evidence to suggest that corticosteroids and IVIg might be beneficial in the postpartum management of MS.
Corticosteroids (methylprednisolone)
In one study, 22 patients from 1996 to 1998 who received no treatment for MS after delivery were compared with 20 patients from 1999 to 2001 who were treated with 1 g of intravenous (IV) corticosteroids monthly for the first 6 months postpartum. Although the mean relapse rate increased during the first 3 months in both groups, it was higher in the untreated group than in the treated group (2 ± 0.66 versus 0.8 ± 0.41).
The finding from this study suggests that prophylactic treatment with IV corticosteroids may be beneficial during the first 3 months after pregnancy. To the authors’ knowledge, however, no studies have adequately assessed the safety of this approach in breastfeeding women.
intravenous immunoglobulin
IVIg treatment may be effective in reducing the incidence of pregnancy- and postpartum-related relapses. Again, the potential risks and benefits must be carefully assessed before treatment is started, especially because the medication falls into category C. Its safety in breastfeeding women is unknown.
In a study of 9 patients with a history of postpartum acute exacerbations of MS who were treated with IVIg for 5 consecutive days in the first week after childbirth and at 6 and 12 weeks afterward, none had a relapse during the 6 months after delivery.
Achiron et al retrospectively studied IVIg treatment during pregnancy and the postpartum period in 108 pregnant patients with relapsing-remitting MS and found a positive effect. The subjects were assigned to an untreated group, a group treated with IVIg in the first week after delivery with booster doses after 6 and 12 weeks, or another group treated continuously with IVIg during and after pregnancy.
Comparison of relapse rates for patients treated with IVIg for the entire pregnancy and relapse rates in the untreated group revealed a positive effect for the former, as follows:
- First trimester – 0.43 versus 0.72
- Second trimester – 0.15 versus 0.61
- Third trimester – 0.0 versus 0.41
- Postpartum period – 0.28 versus 1.33
Relapse rates also decreased in patients treated with IVIg only after delivery (0.58) as compared with untreated patients (1.33). No significant adverse events were associated with IVIg treatment in patients or newborns.
Haas reported that the exacerbation rate after delivery in IVIg-treated individuals was reduced by 33%. IVIg was administered within 3 days after delivery and then monthly to patients thought to be at high risk for exacerbations. They were compared with patients in the PRIMS study, who, for this study, served as control subjects.
Myasthenia Gravis
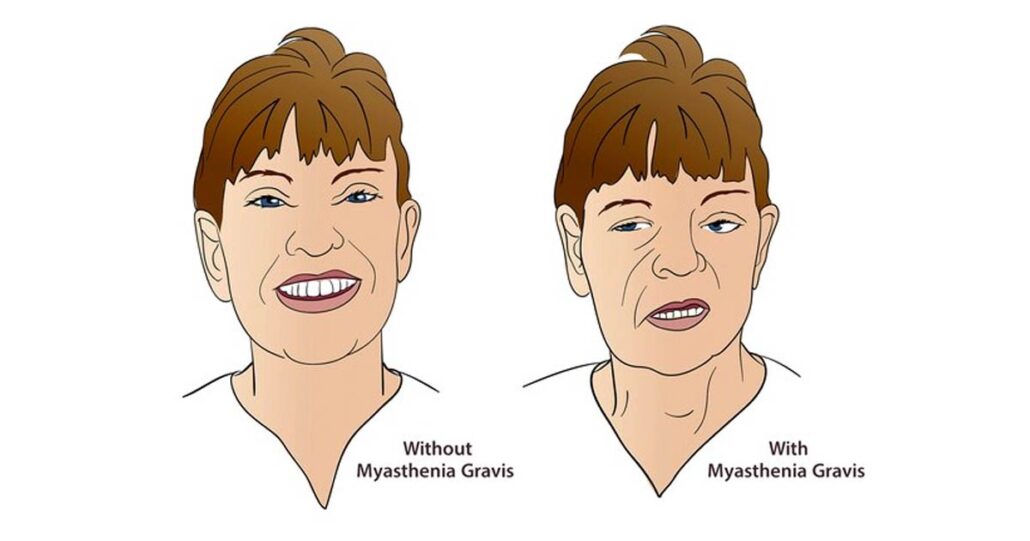
Autoimmune myasthenia gravis (MG) is an uncommon disease of the neuromuscular junction characterized by striated muscle fatigue and weakness. MG frequently affects young women of childbearing age (20-40 years of age), and pregnancy creates potential risks for both the mother and the fetus. (See Myasthenia Gravis and Pregnancy.) During pregnancy, the course of the disease is unpredictable. In a series of 69 pregnancies in 65 women with MG who were treated in a single obstetrics department, 15% had deterioration during pregnancy, and 16% had deterioration during the puerperium. In a report of 64 pregnancies in 47 women with MG, 39% of those treated improved, 42% were unchanged, 19% had deterioration, and 17% of those not receiving therapy had deterioration. Myasthenic symptoms of 28% of women worsened after pregnancy. Therefore, successful management necessarily involves recognizing the potential for myasthenic crisis, optimizing anticholinesterase or immunosuppressive medication treatment, and preparing for the possibility of transient neonatal MG. The challenging care of a woman with MG who is contemplating pregnancy should begin with careful planning and the collaboration of obstetricians and neonatal intensive care specialists. Counseling should address current knowledge, risks, and available treatments. Women with MG who decide to become pregnant should receive prenatal care from providers with experience in treating this disease, and delivery should be performed at a hospital that can manage any complications that may arise.
Management of pregnancy and delivery
The risks and benefits of continuing medication or other immunosuppressive therapy should be discussed, and counseling should begin when the pregnancy is planned. Treatment of MG should be optimized, and clinical improvement should be maximized. The need for immunosuppressant treatment depends on the severity of illness and should be modified according to the duration and severity of the patient’s symptoms of MG. If possible, physicians with experience in treating patients with this disease should perform the delivery at a hospital with the capability to treat both women and infants with complications of MG. In the 1967-2000 Medical Birth Registry of Norway, a population-based cohort study, the potential for cesarean delivery doubled in 127 births by 79 mothers with MG (17.6%) as compared with a reference group (8.6%). The number of births requiring medication to induce labor was not increased. Serious birth defects occurred in 5 children of mothers with MG, but the rate of such defects was not significantly greater than that of a reference group. The preterm rupture of the amniotic membranes was the only complication that occurred more frequently in the MG group than in a comparison group. Rates of neonatal mortality, birth weight, or prematurity did not differ. Pregnancy did not worsen the long-term outcome of MG. Cesarean delivery is recommended if it is necessary for obstetric reasons, and regional anesthesia is safe with correct drug selection. To reduce the potential for adverse effects on the fetus, the immunosuppressive medication should be discontinued if possible, or the dose should be minimized. However, little information about this topic is available in the literature. Some information can be derived from the treatment of patients with other autoimmune disorders but separating the effects from the potential risks of the treated illness is difficult.
Prednisone or prednisolone is associated with a slightly (< 1%) increased risk of cleft palate. High-dose corticosteroids may be associated with premature rupture of amniotic membranes. Methotrexate may be associated with fetal malformations and thus is not recommended for use during childbearing years. Although women taking azathioprine have generally been advised against pregnancy, no teratogenicity or specific malformation pattern has been definitively demonstrated with therapeutic doses in humans.
In a retrospective review of pregnancy outcomes, infants exposed to azathioprine were at risk for the development of reversible leukopenia, anemia, thrombocytopenia, reduced immunoglobulin levels, infection, or thymic atrophy. Babies born to mothers treated with azathioprine have an increased risk of myelosuppression and immunosuppression.
Cyclosporine increases the risk of low birth weight, prematurity, and spontaneous abortions. Nausea and vomiting early in pregnancy may interfere with pyridostigmine dosing. Drug schedules may have to be altered because of increased renal clearance, expanded blood volume, and erratic gastrointestinal absorption.
Discontinuance of maternal immunosuppressants can either worsen or improve MG. If needed, plasma exchange or human intravenous immunoglobulin (IVIg) therapy may be effective and can be safely administered during pregnancy. In theory, plasma exchange can induce premature delivery through large hormonal shifts.
Although MG does not directly affect the uterine smooth muscle, the striated abdominal muscles that contract with the effort of delivery during the second stage of labor may fatigue and weaken more easily than they would if the disease were not present.
Acetylcholinesterase drugs should probably be given parenterally because of their unpredictable oral absorption. Neuromuscular blockers may exaggerate and prolong muscular weakness and should be avoided if possible. Epidural anesthesia is considered relatively safe for vaginal and cesarean deliveries.
Magnesium sulfate is used to prevent seizures in patients with preeclampsia, to treat eclampsia, and to prevent preterm birth in patients with preterm labor; this drug can precipitate weakness by interfering with neuromuscular transmission. Maternal deaths are reported with its use to treat MG in women with preeclampsia.
Consultation with an anesthesiologist should be considered for all pregnant patients with MG.
Complications in newborns

Neonatal MG may result from passive transplacental transfer of antibodies to the nicotinic acetylcholine receptor from the myasthenic mother to the fetus. However, not all infants with detectable levels of antibodies to acetylcholine receptor develop neonatal MG.
The severity of symptoms varies, ranging from mild hypotonia to respiratory distress. Clinical symptoms develop in the first few hours after birth and usually resolve within 2-3 weeks. In the Medical Birth Registry of Norway, 21.3% of children of mothers with MG needed transfer to intensive care units (ICUs), compared with 2% of the reference group. Other studies have shown a neonatal MG incidence of 10-21%, and neonatal disease was reported in 4% (but probably affected 12%) of the Norway registry cohort.
Children of mothers with MG require careful observation in the first few days after birth, and symptoms may respond to anticholinesterase medication. Women with MG should deliver in a facility with a neonatal ICU.
Arthrogryposis multiplex congenita, characterized by multiple joint contractures in utero, occasionally complicates the pregnancy of a mother with MG. Circulating antibodies may inhibit the function of fetal acetylcholine receptors, with little effect on adult acetylcholine receptor function, and may be responsible for this condition.
A high ratio of antifetal to antiadult muscle antiacetylcholine receptor antibodies is predictive of neonatal MG in the first child of a mother with the disease. Elevated alpha-fetoprotein levels may inhibit acetylcholine antibody binding capacity, and this may explain the delay to onset of neonatal MG symptoms after birth.
Cerebrovascular Disease
Stroke is the third leading cause of death and the primary cause of adult disability in the United States. It may be broadly classified as either ischemic or hemorrhagic. Although the cerebrovascular disease is thought to be uncommon in pregnancy, it is an important source of maternal and fetal morbidity and mortality, causing 3.5-26 cases of neurologic dysfunction per 100,000 deliveries, and is associated with more than 12% of maternal deaths.
The incidence of stroke during the childbearing ages alone is 10.7 cases per 100,000 women. Some authors have questioned whether the risk of stroke increases in association with pregnancy itself; however, evidence suggests that the postpartum period is associated with an increased risk of ischemic stroke.
Ischemic stroke
Ischemic strokes account for 85% of all strokes. Causes of ischemic stroke in pregnancy may be divided into 2 general categories: pregnancy-specific etiologies and stroke-in-the-young factors.
The first category includes the following:
- Preeclampsia and eclampsia – These are present in 24-47% of ischemic strokes and 14-44% of intracranial hemorrhages
- Choriocarcinoma
- Amniotic fluid embolism
- Peripartum cardiomyopathy
- Postpartum cerebral angiopathy – This rare and reversible condition causes narrowing of the blood vessels, which can lead to ischemia
Causes of stroke in a young person include the following:
- Atherothrombotic etiologies
- Cardioembolic events
- Lacunar disease
- Other vasculopathy (e.g., fibromuscular dysplasia [FMD], dissection, or arteritis)
- Hematologic disorders
- Drugs (e.g., cocaine)
- Migraine
- Unknown causes
Some causes in this category are less common in stroke than in other settings; they occur most frequently in relatively young women.
Lupus
The systemic lupus erythematosus (SLE) is one of the disorders that is most common in women. SLE is associated with cerebrovascular events arising from hypercoagulability associated with antiphospholipid antibodies or vasculitis. Thrombus may have a cardiac origin or may come from within the intracranial vasculature.
Antiphospholipid antibody syndrome and hypercoagulable states
Antiphospholipid antibody syndrome is associated with stroke in young women and with SLE and other collagen-vascular diseases. The patient’s medical history is important for diagnosing the disorder and should include a pertinent history of spontaneous abortions or intrauterine fetal demise (especially if multiple), thrombotic events, a family history of stroke or antiphospholipid antibody syndrome, and thrombocytopenia. Treatment usually consists of anticoagulation. Other hypercoagulable states that occur in young women include the following:
- Antithrombin III deficiency
- Protein C or S deficiencies
- Resistance to activated protein C
- Dysfibrinogenemia
- Homocystinemia
- Plasminogen and plasminogen-activator deficiency
Because pregnancy itself results in a hypercoagulable state, the risk for thrombotic events increases in patients with a known preexisting hypercoagulable condition. These disorders should also be considered in young women with stroke and should be investigated if suspected.
Vasculopathy
Vasculitis is a rare condition that may occur in women of childbearing age and may result in stroke if it involves the cerebral vessels. In addition to focal symptoms of ischemia (stroke), cerebral vasculitis may cause nonfocal symptoms such as headache and encephalopathy. If suspected, particularly in the setting of known systemic vasculitis, the patient should be evaluated with appropriate laboratory and imaging studies. Primary central nervous system (CNS) vasculitis is extremely rare.
Other forms of vasculopathy have been related to stroke in females of childbearing age. This category of noninflammatory vascular disease includes the following:
- FMD
- Arterial dissection
- Moyamoya disease
Arterial dissection causes symptoms of stroke secondary to embolic fragments from the dissection site. Potential causes of a dissection include FMD, trauma, hypertension, and spontaneous etiologies. Treatment for vasculopathy is disease-specific and may involve anticoagulation or surgical intervention.
Migraine headaches are common in young women and can be associated with stroke, but these instances are rare. It is a diagnosis of exclusion.
Cerebral venous thrombosis
Cerebral venous thrombosis (CVT) can cause symptoms of focal dysfunction that mimic those of ischemic stroke. Because of the hypercoagulable state during pregnancy, CVT is more common currently than at others. The postpartum period has the highest risk for CVT. One study demonstrated that the risk of intracranial venous thrombosis was 11.66 cases per 100,000 deliveries. Treatment of CVT usually consists of anticoagulation and close monitoring.
Drug use
Use and abuse of legal and illegal drugs have also been associated, probably causally, with ischemic stroke and intracerebral hemorrhage. The drugs most specifically related to strokes include the following:
- Ephedrine
- Pseudoephedrine
- Phenylpropanolamine
- Heroin
- Cocaine
- Amphetamines
- Alcohol
These drugs may cause stroke by means of several mechanisms (e.g., hypertensive surges, arterial vasospasm, arrhythmias, hypercoagulopathy, and embolization of diluent particles). Treatment should be focused on stopping use of the drug and on rehabilitation.
Hemorrhagic stroke
Women at risk for intracerebral hemorrhage in pregnancy are those with eclampsia, vasculitis, or an aneurysm or vascular malformation. High blood pressure is the most important risk factor for intracranial hemorrhage in pregnancy. Prevention is the key. Blood pressure should be monitored closely during pregnancy.
Clinical evaluation
History and physical examination
Obtaining a history and performing a physical examination are important aspects of evaluating the type of cerebrovascular event that may have occurred. Important historical points include pain (e.g., headache or neck pain), trauma, fluctuating neurologic symptoms, seizures, mental status changes, recent fevers, and drug use.
A complete history should include a medical history of previous stroke or risk factors for stroke, spontaneous abortions, collagen vascular disease, and family history. In addition, a history of complications that developed during the current and previous pregnancies should be obtained. The patient should undergo a complete physical examination, including funduscopic, cardiovascular, skin, and full neurologic examinations.
Diagnostic imaging
Imaging studies are required, and several options are available. Computed tomography (CT) is the most useful study for ruling out acute hemorrhage; it is also useful for evaluating ischemic stroke. CT angiography (CTA) and CT venography (CTV) can also be useful for evaluating the cerebral vasculature. CT studies produce results quickly, but they also pose a small radiation risk to the fetus. Evaluation of bleeding from ruptured intracranial aneurysms or arteriovenous malformations (AVMs) may require extensive imaging, including cerebral arteriography.
Magnetic resonance imaging (MRI) is useful for evaluating stroke in a pregnant patient. It does not carry the risk of radiation exposure, and the contrast material required for some studies is associated with few reports of adverse reactions, unlike the contrast material used for CT studies. Although MRI takes longer to perform than CT does, it offers a more detailed view of the brain tissue (especially the posterior fossa). In addition, the diffusion-weighted images allow greater accuracy in the diagnosis of acute ischemic events.
Other diagnostic studies that may be used to evaluate a patient with ischemic stroke include carotid Doppler imaging, transesophageal (TEE) or transthoracic echocardiography (TTE), electrocardiography (ECG), and, occasionally, transcranial Doppler imaging.
Laboratory tests
The choice of laboratory studies depends on the mechanism of the stroke and on whether the arterial or the venous system is involved. Studies may include the following:
- Hemoglobin electrophoresis
- Fasting homocysteine level determination
- Cholesterol panel
- Anticardiolipin or antiphospholipid antibody tests
- Thrombin time determination for dysfibrinogenemia and for factor V Leiden
- Prothrombin G20210A mutation tests
- Protein C or S tests – Note that protein S activity is decreased during pregnancy; if possible, the protein study should be performed 6-8 weeks after delivery
- Antithrombin III assays
Other studies may be indicated to investigate for SLE, other causes of vasculitis, and other systemic diseases.
Differential diagnosis
The differential diagnosis of stroke in young women includes seizure, brain tumor, reversible posterior leukoencephalopathy (RPLE), multiple sclerosis (MS), and migraine. In appropriate settings, infectious causes (e.g., Lyme disease and bacterial endocarditis) should be considered.
Treatment
Treatment of stroke may minimize neuronal damage and is aimed at preventing recurrences. In pregnancy, factors such as maternal risk versus expected benefit and the level of fetal risk must be considered. The stroke etiology also must be considered when determining the best treatment.
Ischemic stroke
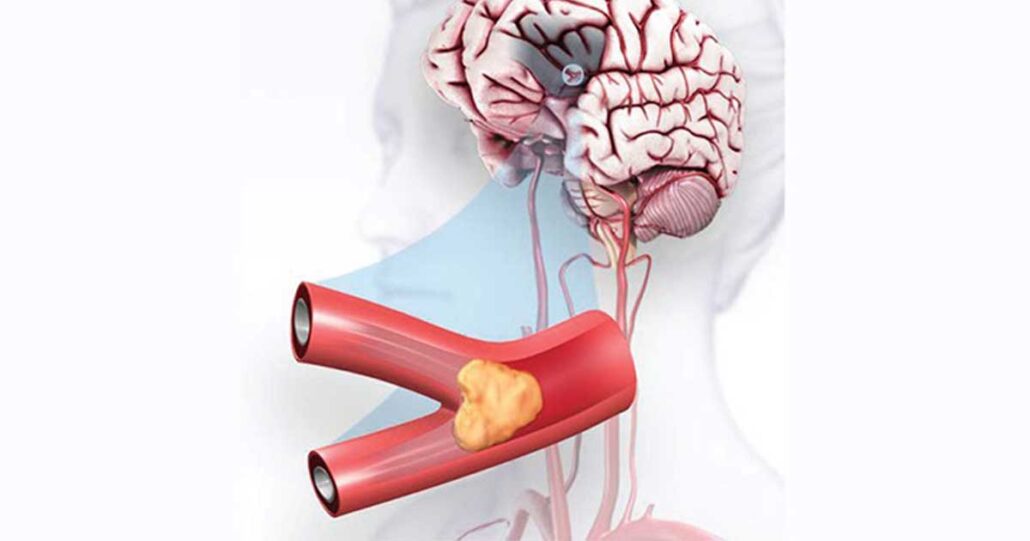
Tissue-type plasminogen activator (tPA) is a category C agent in pregnancy. Its effects on humans and animals during pregnancy have not been adequately evaluated, and at this point, it is contraindicated. However, recent reports of its use have led to reconsideration of this position. TPA is a large molecule (7200kDa) and does not cross the placental barrier. There are no teratogenic effects in short-term studies in animals, no tumorigenicity in rodents, no mutagenicity or production of chromosomal aberrations in human lymphocytes, and in rabbits no maternal or fetal toxicity at 1mg/kg dosage. Three publications reporting on treatment of 8 mothers provided encouraging outcome data. There was good neurological recovery in most mothers. One patient also had IA angioplasty, which led to dissection, a malignant MCA infarct, and death. One patient sustained an intrauterine hematoma that was drained. Fetal outcome in 5 babies was good. In two early cases medical termination of pregnancy was opted for, and one child died with the mother.
The current recommendations, based on expert opinion,are that treatment decisions should be made balancing the natural history – prognosis without tPA treatment and the benefit of treatment – taking into consideration the risks of treatment.
Use of IV tPA can be considered in a pregnant patient. The chief risk to the mother is a symptomatic intracranial bleed, which is lower in individuals < 60 years: 2.8%, and a bleed elsewhere. To date, there has not been a demonstrated risk to the fetus with IV tPA. Despite in vitro concerns, iodinated contrast seems safe to use during pregnancy. IV contrast does not pose a risk to the fetus.
Although other interventional techniques are being developed to treat acute stroke, information about treating the pregnant patient with stroke with these modalities is limited. When any of these modalities is considered in a pregnant woman, the known risks of withholding treatment must be balanced against the unknown risks of treatment.
The stage of the pregnancy (i.e., the gestational age) likely factors into the considerations. From a dosing standpoint, targeted intra-arterial treatment might be safer than other routes, but it presents radiation risks to the fetus because of the use of x-ray fluoroscopy during the treatment.
The major categories of medications used in stroke prophylaxis are anticoagulants and antiplatelet agents. Their safety profiles during pregnancy vary as follows:
- Aspirin – Category D (but a low dose is relatively safe)
- Clopidogrel – Category B
- Dipyridamole – Category B (but the aspirin-dipyridamole combination is category D)
- Heparin and heparinlike compounds – Category C
- Warfarin – Category X
Heparin is routinely used during pregnancy when anticoagulation is needed because it does not cross the placenta. It takes effect quickly and can be stopped abruptly. Associated risks and adverse reactions include heparin-induced thrombocytopenia, osteoporosis (with the use of low-molecular-weight heparin or unfractionated heparin), and bleeding.
Warfarin crosses the placenta and can cause complications with organogenesis (i.e., during weeks 6-12 of gestation). Maternal-fetal bleeding can occur with warfarin, as can spontaneous abortions and stillbirths.
Aspirin can result in fetal complications if given for prolonged periods in high doses; therefore, it is not used for long-term treatment with an antithrombotic agent in pregnancy. Adverse events appear to be dose-related; hence, studies have used a low dose (60 mg), which was not strongly associated with pregnancy-related complications.
Use of clopidogrel in human pregnancies has not been adequately studied. Dipyridamole is also a category B drug in pregnancy. Dipyridamole has not caused clinically significant teratogenic effects in animals when given in moderate doses; further studies of its safety must be performed. The aspirin-dipyridamole combination has limited use in pregnancy because of the adverse effects of aspirin.
Hemorrhagic stroke
Management of hemorrhagic stroke depends on its location and etiology. General measures include discontinuance of antithrombotics or anticoagulation, management of blood pressure, and general supportive measures. Ruptured cerebral aneurysms or AVMs that have bled may have to be treated urgently either with open surgery or with endovascular interventions.
It is easiest to proceed with these treatment decisions if all parties agree that the life of the mother takes precedence. When treatment is optimized for the mother, it may be impossible to safeguard the fetus from all risks.
Prevention of stroke
All women may decrease their risk of stroke by avoiding smoking, by maintaining a healthy body mass index, by avoiding excess alcohol use, by avoiding use of all illegal drugs, and by having their blood pressure checked periodically to detect hypertension. If they are at particular risk for diabetes or elevated cholesterol levels, periodic checks by their primary healthcare provider may be indicated. If hypertension, diabetes, or hypercholesterolemia is diagnosed, meticulous treatment lowers the risk of stroke.
Women with known cerebrovascular disease who are pregnant or plan to become pregnant may take steps to maximize the safety of their pregnancy. If they have previously experienced a cerebral infarction, its cause should have been or should be determined, preferably before the pregnancy occurs, so that appropriate measures can be instituted to minimize the risk of recurrence.
In patients with a known cerebral aneurysm, clipping or coiling should be performed, if possible. Consider cesarean delivery. In patients with a known AVM, the lesion should be resected or embolized. The preferred mode of delivery has not been established.
Opinions differ regarding the best approach to treating pregnant women with hypercoagulable states (thrombophilia). Some authors reserve anticoagulant treatment for those with severe thrombophilias by considering the specific etiology and past clinical symptoms, particularly those noted during previous pregnancies. Patients who previously took warfarin because of recurrent venous thrombotic events must be switched to heparin or a heparinoid before conceiving; this anticoagulant regimen should be maintained throughout the pregnancy.
Some authorities add low-dose aspirin to manage relatively severe thrombophilias. Decisions regarding treatment of mild or moderate thrombophilias must be individualized; some authors reserve the use of anticoagulation for the peripartum period.



