Epidural Hematoma
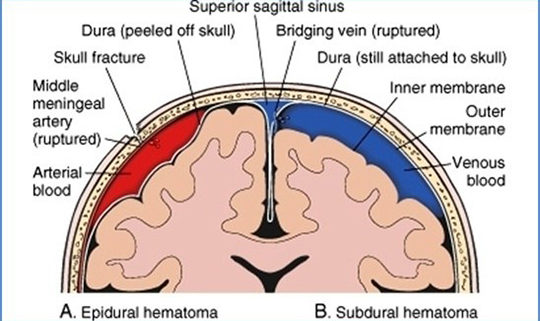
Epidural hematoma (i.e., accumulation of blood in the potential space between dura and bone) may be intracranial (EDH) or spinal (SEDH). Intracranial epidural hematoma occurs in approximately 2% of patients with head injuries and 5-15% of patients with fatal head injuries. Intracranial epidural hematoma is considered to be the most serious complication of head injury, requiring immediate diagnosis and surgical intervention. Intracranial epidural hematoma may be acute (58%), subacute (31%), or chronic (11%). Spinal epidural hematoma may also be traumatic, though it may occur spontaneously.
Pathophysiology
Epidural hematoma usually results from a brief linear contact force to the calvaria that cause separation of the periosteal dura from bone and disruption of interposed vessels due to shearing stress. Skull fractures occur in 85-95% of adult cases, but they are much less common in children because of the plasticity of the immature calvaria. Arterial or venous structures may be compromised, causing rapid expansion of the hematoma; however, chronic or delayed manifestations may occur when venous sources are involved. Extension of the hematoma usually is limited by suture lines owing to the tight attachment of the dura at these locations. Recent analyses have revealed that epidural hematomas may actually traverse suture lines in a minority of cases.
The temporoparietal region and the middle meningeal artery are involved most commonly (66%), although the anterior ethmoidal artery may be involved in frontal injuries, the transverse or sigmoid sinus in occipital injuries, and the superior sagittal sinus in trauma to the vertex. Bilateral epidural hematomas account for 2-10% of all acute epidural hematomas in adults but are exceedingly rare in children. Posterior fossa epidural hematomas represent 5% of all cases of epidural hematomas.
Spinal epidural hematoma may be spontaneous or may follow minor trauma, such as lumbar puncture or epidural anesthesia. Spontaneous spinal epidural hematoma may be associated with anticoagulation, thrombolysis, blood dyscrasias, coagulopathies, thrombocytopenia, neoplasms, or vascular malformations. The peridural venous plexus usually is involved, though arterial sources of hemorrhage also occur. The dorsal aspect of the thoracic or lumbar region is involved most commonly, with expansion limited to a few vertebral levels.
Epidemiology
Frequency
United States
Epidural hematoma complicates 2% of cases of head trauma (approximately 40,000 cases per year). Spinal epidural hematoma affects 1 per 1,000,000 people annually. Alcohol and other forms of intoxication have been associated with a higher incidence of epidural hematoma.
International
International frequency is unknown, though it is likely to parallel the frequency in the United States.
Mortality/Morbidity
Mortality rate associated with epidural hematoma has been estimated to be 5-50%.
-The level of consciousness prior to surgery has been correlated with mortality rate: 0% for awake patients, 9% for obtunded patients, and 20% for comatose patients.
-Bilateral intracranial epidural hematoma has a mortality rate of 15-20%.
-Posterior fossa epidural hematoma has a mortality rate of 26%.
Race
No racial predilection has been reported.
Sex
Intracranial and spinal epidural hematomas are more frequent in men, with a male-to-female ratio of 4:1.
Age
See the list below:
- Intracranial epidural hematoma is rare in individuals younger than 2 years.
- Intracranial epidural hematoma is also rare in individuals older than 60 years because the dura is tightly adherent to the calvaria.
- Spinal epidural hematoma has a bimodal distribution with peaks during childhood and during the fifth and sixth decades of life. Increasing age has been noted as a risk factor for postoperative spinal epidural hematoma.
Epidural Hematoma Clinical Presentation
History
Epidural hematoma should be suspected in any individual who sustains head trauma. Although classically associated with a lucid interval between the initial loss of consciousness at the time of impact and a delayed decline in mental status (10-33% of cases), alterations in the level of consciousness may have a variable presentation. Posterior fossa epidural hematoma may exhibit a rapid and delayed progression from minimal symptoms to even death within minutes.
Symptoms of epidural hematoma include the following:
- Headache
- Nausea/vomiting
- Seizures
- Focal neurologic deficits (e.g., visual field cuts, aphasia, weakness, numbness)
Spinal epidural hematoma typically causes severe localized back pain with delayed radicular radiation that may mimic disk herniation. Associated symptoms may include the following:
- Weakness
- Numbness
- Urinary incontinence
- Fecal incontinence
Physical
See the list below:
The physical examination should include a thorough evaluation for evidence of traumatic sequelae and associated neurological deficits, including the following:
- Bradycardia and/or hypertension indicative of elevated intracranial pressure
- Skull fractures, hematomas, or lacerations
- Cerebrospinal fluid (CSF) otorrhea or rhinorrhea resulting from skull fracture with disruption of the dura
- Hemotympanum
- Instability of the vertebral column
- Alteration in level of consciousness (i.e., Glasgow Coma Scale score; see the Glasgow Coma Scale calculator)
- Anisocoria (e.g., ipsilateral dilation of the pupil due to uncal herniation with compression of the oculomotor nerve)
- Facial nerve injury
- Weakness (e.g., contralateral hemiparesis due to compression of the cerebral peduncle)
- Other focal neurological deficits (e.g., aphasia, visual field defects, numbness, ataxia)
Spinal epidural hematoma may have variable findings on physical examination, determined by the level of the lesion. The findings include the following:
- Weakness (unilateral or bilateral)
- Sensory deficits with radicular paresthesias (unilateral or bilateral)
- Various alterations in reflexes
- Alterations of bladder or anal sphincter tone
Causes
See the list below:
- Trauma
- Anticoagulation
- Thrombolysis
- Lumbar puncture
- Epidural anesthesia
- Coagulopathy or bleeding diathesis
- Hepatic disease with portal hypertension
- Cancer
- Vascular malformation
- Disk herniation
- Paget disease of bone
- Valsalva maneuver
- Hypertension
- Chiropractic manipulation
Differential Diagnoses
- Alcohol (Ethanol) Related Neuropathy
- Anisocoria
- Diagnosis and Management of Cervical Spondylosis
- Foix-Alajouanine Syndrome
- Head Injury
- Imaging in Ankylosing Spondylitis
- Intracranial Epidural Abscess
- Intracranial Hemorrhage
- Posttraumatic Epilepsy
- Spinal Cord Hemorrhage
- Spinal Epidural Abscess
Laboratory Studies
See the list below:
- Complete blood count (CBC) with platelets – To monitor for infection and assess hematocrit and platelets for further hemorrhagic risk.
- Prothrombin time (PT)/activated partial thromboplastin time (aPTT) – To identify bleeding diathesis.
- Serum chemistries, including electrolytes, blood urea nitrogen (BUN), creatinine, and glucose – To characterize metabolic derangements that may complicate clinical course.
- Toxicology screen and serum alcohol level – To identify associated causes of head trauma and establish need for surveillance with regard to withdrawal symptoms.
- Type and hold an appropriate amount of blood – To prepare for necessary transfusions needed because of blood loss or anemia.
Imaging Studies
See the list below:
- Plain radiography of the head (skull radiography) may reveal skull fractures, though CT scanning has largely replaced the use of skull radiography because the diagnostic information is so much greater with CT. Cervical spine radiographs with anteroposterior, lateral, and odontoid views are useful to identify associated traumatic fractures. Plain radiographs of the vertebral column may identify a cavernous angioma.
- Myelography outlines the epidural space and may illustrate a space-occupying mass. CT myelography may be used when MRI is unavailable or if the patient cannot tolerate MRI.
- Noncontrast CT scanning of the head not only visualizes skull fractures but also directly images an epidural hematoma.
- Acute epidural hematoma may appear as a hyperdense lenticular-shaped mass situated between the brain and the skull, though regions of hypodensity may be seen with serum or fresh blood. On rare occasion, an acute epidural may appear completely isointense with respect to brain. Planoconvex or crescent-shaped epidural hematoma must be differentiated from subdural hemorrhage. Subdural hematomas may rarely appear convex and mimic epidural hematomas. Subacute lesions are homogenously hyperdense.
- Chronic epidural hematoma may have a heterogeneous appearance due to neovascularization and granulation, with peripheral enhancement on contrast administration.
- CT scanning may also depict air collections and displacement of brain parenchyma.
- Clinical deterioration should prompt repeat imaging with CT scanning.
MRI also demonstrates the evolution of an epidural hematoma, though this imaging modality may not be appropriate for patients in unstable condition.
- Spinal MRI may delineate the location of an epidural hematoma and identify an associated vascular malformation.
- Spinal cord enhancement may be apparent and should be distinguished from inflammation or neoplasia.
- Diffusion-weighted imaging with the use of periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER) MRI may be used for improved detection of acute spinal epidural hematoma.
- Gadolinium-enhanced magnetic resonance arteriography (MRA) may further define the extent of an arteriovenous malformation.
- Conventional angiography may be required to demonstrate definitively the presence of a vascular malformation.
Other Tests
Functional studies of the spinal cord, such as somatosensory evoked potentials, may be used for intraoperative monitoring or for prognostication following surgery.
Procedures
See the list below:
- Emergent decompression with placement of a burr hole may be necessary when neurosurgical consultation is unavailable. For patients showing rapid deterioration with clinical signs of impending herniation, place a burr hole on the side of the dilating pupil. In the absence of a CT scan, place the burr hole 2- finger widths anterior to the tragus of the ear and 3 finger widths above the tragus of the ear.
- Lumbar puncture provides little additional information and may exacerbate neurologic damage.
Medical Care
Initial resuscitation efforts should include assessment and stabilization of airway patency, breathing, and circulation. A thorough trauma evaluation is mandatory, including inspection for skull fractures and appreciation of the force and location of impact. Immobilization of the spine should be followed by emergent transfer of the patient to the nearest level I trauma center supported with neurosurgical consultation.
- Triage and initial management of a patient with epidural hematoma may be tailored to the degree of neurological impairment at presentation. Alert patients may be evaluated with a CT scan following a brief neurologic examination.
- A patient with a small epidural hematoma may be treated conservatively, though close observation is advised, as delayed, yet sudden, neurological deterioration may occur.
- Trauma patients may require diagnostic peritoneal lavage and radiographs of the chest, pelvis, and cervical spine.
- While neurosurgical consultation is requested, administer intravenous fluids to maintain euvolemia and to provide adequate cerebral perfusion pressure.
- Patients with elevated intracranial pressure may be treated with osmotic diuretics and hyperventilation, with elevation of the head of the bed at an angle of 30 degrees. Patients who are intubated may be hyperventilated with intermittent mandatory ventilation at a rate of 16-20 breaths per minute and tidal volume of 10-12 mL/kg. A carbon dioxide partial pressure of 28-32 mm Hg is ideal, as severe hypocapnia (< 25 mm Hg) may induce cerebral vasoconstriction and ischemia.
- Coagulopathy or persistent bleeding may require administration of vitamin K, protamine sulfate, fresh frozen plasma, platelet transfusions, or clotting factor concentrates.
Surgical Care
Although several recent reports have described successful conservative management of epidural hematoma, surgical evacuation constitutes definitive treatment of this condition. Craniotomy or laminectomy is followed by evacuation of the hematoma, coagulation of bleeding sites, and inspection of the dura. The dura is then tented to the bone and, occasionally, epidural drains are employed for as long as 24 hours.
See the list below:
- Minimally invasive surgical procedures, including the use of burr holes and negative pressure drainage, may be used in selected cases
- Endovascular embolization to minimize bleeding during the acute stage
- Thrombolytic evacuation using closed suction drain
- Novel therapeutic approaches
Consultations
See the list below:
- Neurosurgeon (for potential emergent evacuation of the hematoma)
- Neurologist
- Rehabilitation specialist
Diet
The hypermetabolic and catabolic phenomena associated with severe head injury necessitate caloric supplementation. Initiate enteral feedings as soon as possible.
Activity
Patients who are treated conservatively should undergo close observation and should avoid strenuous activity. Inpatients should remain on bedrest during the initial phase; this can be followed by a progressive increase in activity.

Epidural-Hematoma
Medication Summary
Osmotic diuretics, such as mannitol or hypertonic saline, may be used to diminish intracranial pressure. As hyperthermia may exacerbate neurological injury, acetaminophen may be given to reduce fevers. Anticonvulsants are used routinely to avoid seizures that may be induced by cortical damage. Patients with spinal epidural hematoma may require high-dose methylprednisolone when spinal cord compression is involved. Immobilized patients may require heparin for prevention of venous thrombosis, whereas vitamin K and protamine may be administered to restore normal coagulation parameters. Antacids are used to prevent gastric ulcers associated with traumatic brain injury and spinal cord damage.
Osmotic diuretics
Class Summary
These agents reverse the pressure gradient across the blood-brain barrier, reducing intracranial pressure.
Mannitol (Osmitrol, Resectisol)
Reduces cerebral edema by osmotic forces and decreases blood viscosity, resulting in reflex vasoconstriction and lowering of intracranial pressure.
Antipyretic agents
Class Summary
These agents are helpful in relieving the fever associated with the condition.
Acetaminophen (Tylenol, Feverall, Aspirin Free Anacin)
Reduces fever and maintains normothermia. DOC for pain in patients with documented hypersensitivity to aspirin or NSAIDs, with upper GI disease, or who are taking oral anticoagulants.
Anticonvulsants
Class Summary
These agents reduce frequency of early posttraumatic seizures from 14% to 4%, but they do not prevent later seizures. If seizures are not experienced for 7-10 d, the drug may be discontinued.
Fosphenytoin (Cerebyx)
Converted to phenytoin, which modulates neuronal voltage-dependent sodium channels.
Corticosteroids
Class Summary
Anti-inflammatory properties mitigate tissue damage in spinal cord compression.
Methylprednisolone (Adlone, Medrol, Solu-Medrol)
Reduces injury associated with spinal cord compression. Decreases inflammation by suppressing migration of polymorphonuclear leukocytes and reversing increased capillary permeability.
Antidotes
Class Summary
These agents reverse some coagulopathies or bleeding diatheses.
Phytonadione; vitamin K (AquaMEPHYTON, Konakion, Mephyton)
Promotes hepatic synthesis of clotting factors that inhibit warfarin effects.
Protamine
Neutralizes effects of heparin.
Antacids
Class Summary
These agents provide prophylaxis of gastric ulcers.
Famotidine (Pepcid)
Competitively inhibits histamine at H2 receptor of gastric parietal cells, resulting in reduced gastric acid secretion, gastric volume, and hydrogen concentrations. Minimizes development of gastric ulcers.
Anticoagulants
Class Summary
These agents reduce risk of venous complications in immobilized patients.
Heparin
Augments activity of antithrombin III and prevents conversion of fibrinogen to fibrin. Does not actively lyse but is able to inhibit further thrombogenesis. Prevents re-accumulation of clot after spontaneous fibrinolysis. Used for prophylaxis of deep venous thrombosis.
Further Outpatient Care
After hospital discharge, continued physical, occupational, and speech therapy may be required.
Further Inpatient Care
Following initial management in the emergency department, the patient may be sent for emergent neurosurgical evacuation of the hematoma or may be transferred to the ICU for further care. Subsequent care generally includes the following:
- Serial neurologic examinations
- Treatment of elevated intracranial pressure
- Avoidance of hypotension or hypertension (i.e., maintain mean arterial pressure [MAP] between 70-130 mm Hg)
- Use of isotonic solutions, such as normal saline, to minimize cerebral edema
- Avoidance of hyperthermia
- Treatment or prevention of posttraumatic seizures
- Observation and potential repair of CSF leaks
- Treatment of urinary tract infections
- Prevention of venous thrombosis
- Prophylaxis for gastric ulcers
- Physical, occupational, and speech therapy
- Repeat CT scan for clinical deterioration
Inpatient & Outpatient Medications
See the list below:
- Mannitol or other osmotic diuretics for elevated intracranial pressure
- Steroids for spinal cord compression
- Subcutaneous heparin for prevention of venous complications
- Famotidine or other antacids for gastric ulcer prophylaxis
- Fosphenytoin or other anticonvulsants for posttraumatic seizures
- Anticholinergics for bladder complications
- Baclofen, diazepam, or tizanidine for spasticity due to spinal cord damage
- Amitriptyline, carbamazepine, or gabapentin for neuropathic pain
- Acetaminophen for fever
Transfer
Although emergent decompression of an epidural hematoma should not be delayed, trauma patients should be transferred to centers with neurosurgical expertise.
Deterrence/Prevention
See the list below:
- Educate the public regarding traumatic brain injury, including appropriate use of safety equipment, precautions, and measures that may reduce the incidence of head injury.
- Avoid lumbar puncture or epidural anesthesia in individuals on anticoagulation, following thrombolysis, or when a bleeding diathesis is suspected.
Complications
See the list below:
- Neurological deficits or death may occur.
- Posttraumatic seizures due to cortical damage may develop 1-3 months after the initial injury, with decreasing frequency over time. Alcoholism increases the risk of posttraumatic seizures.
- Delayed effects of an epidural hematoma include the postconcussion syndrome, which is characterized by headaches, dizziness, vertigo, restlessness, emotional lability, inability to concentrate, and fatigue.
- Spinal epidural hematoma may cause spasticity, neuropathic pain, and urinary complications.
Prognosis
See the list below:
- Declines with advancing age
- Deteriorates when associated with other intracranial injuries
- Depends on the initial Glasgow Coma Scale score (0% mortality for awake patients, 40% mortality for comatose individuals)
- Worsens with delays between injury and surgical intervention
- In spinal epidural hematoma, the MRI appearance of T2-hyperintensity within the spinal cord may portend a poor clinical outcome.
Patient Education
Educate patients regarding prevention of traumatic brain injury, with particular emphasis on sports injuries, use of safety precautions, and proper use of safety equipment.


Leave a Reply
Want to join the discussion?Feel free to contribute!