Major Depressive Disorder (MDD) or Clinical Depression
What is major depressive disorder (MDD) or clinical depression?
Major depressive disorder (MDD) or clinical depression is the leading cause of mental disorders worldwide. The WHO estimates that more than 300 million people suffer from MDD. About 75% of people with mental disorders remain untreated in developing countries, with almost 1-million people taking their lives each year.
In the United States, the Centers for Disease Control and Prevention (CDC) estimates that MDD affects more than 16.2 million American adults, ages 18 and over in any given year. While MDD can develop at any age, the median age at onset is 32.5 years old. MDD is more prevalent in women than in men.
Sadness and grief are normal human emotions. We all have those feelings from time to time, but they usually go away within a few days. MDD or clinical depression, however, is a serious mood disorder and can bring about long-lasting symptoms such as overwhelming sadness, low energy, loss of appetite, and a lack of interest in things that used to bring pleasure.
MDD can get worse over time without proper treatment. People usually are not able to just get over a depressive state. For some, MDD may be a lifelong challenge that requires treatment on a long-term basis. Those who seek treatment see improvements in symptoms in just a few weeks and will go on to live healthy and happy lives.
If left untreated, MDD can lead to serious health complications, including suicide. Fortunately, there are effective treatments for MDD through options like therapy, medication, diet, and exercise.
Determining if persistent, unshakable dark feelings are a result of MDD can be the first step toward healing and recovery. Read through these warning signs to see if it is time for you to see a mental health professional.
Types of clinical depression
MDD can be categorized depending on the severity of symptoms. Some people experience mild and temporary episodes, while others experience severe and ongoing depressive episodes.
There are two main types: major depressive disorder (MDD) and persistent depressive disorder. Specific circumstances can trigger other forms of clinical depression or subsets of the condition.

Major depressive disorder or clinical depression
A major depressive disorder is the more severe form of clinical depression that is characterized by persistent feelings of sadness, hopelessness, and worthlessness that do not go away on their own.
The diagnosis requires five or more of the following symptoms over a 2-week period:
- Feeling depressed most of the day
- Loss of interest in most regular activities
- Significant weight loss or gain
- Sleeping a lot or not being able to sleep
- Slowed thinking or movement
- Fatigue or low energy most days
- Feelings of worthlessness or guilt
- Loss of concentration or indecisiveness
- Recurring thoughts of death or suicide
There are different subtypes of major depressive disorder, which the American Psychiatric Association refers to as “specifiers.”
These include:
- Atypical features
- Anxious distress
- Mixed features
- Peripartum onset, during pregnancy or right after giving birth
- Seasonal patterns
- Melancholic features
- Psychotic features
- Catatonia
Persistent depressive disorder
Persistent depressive disorder (PDD) used to be called dysthymia. It is a milder but chronic form of MDD. The diagnosis requires that symptoms last for at least 2-years. It occurs in 1.5 percent of U.S. adults annually. It is more prevalent in women than men, and half of all cases are serious.
The following are often present in people with PDD:
- Loss of interest in normal daily activities
- Hopelessness
- Deep sadness
- Lack of productivity
- Low self-esteem
- Low energy
- Indecisiveness
Bipolar disorder
Another type of clinical depression is bipolar disorder or manic-depressive disorder. It affects about 2.8 percent of the U.S. population each year. It occurs equally in men and women, while 83 percent of cases are considered severe.
The disorder involves manic or energized mood episodes. Sometimes, these may be preceded or followed by episodes of clinical depression. The presence of these episodes determines the type of bipolar disorder.
Psychotic depression
When major depression or bipolar disorder are accompanied by hallucinations, delusions, or paranoia, it is called major depressive disorder with psychotic features. About 25-percent of patients have psychotic depression. 1 in 13 people worldwide will experience a psychotic episode before age 75.
Seasonal
If you have a major depressive disorder with a seasonal pattern, also known as a seasonal affective disorder, your mood is affected by seasonal changes. As daylight hours get shorter in the winter, many people develop feelings of lethargy, tiredness, and a loss of interest in everyday activities. Your doctor may prescribe medication or a lightbox to help treat this condition. The condition usually goes away once the days get longer.
Geography and distance from the equator play significant roles in this disorder. Women also represent 4 out of 5 people with the condition.
Situational
Losing a loved one or a job, financial troubles, or a sudden change in circumstances can have an impact on people and trigger depression.
Common symptoms of depression
Symptoms of depression can vary. They may manifest themselves differently from person to person. However, for most people, depression symptoms affect their ability to perform daily activities, interact with others, or go to work or go to school. If you suffer from depression, you may often experience several of the following:
Increased fatigue and sleep problems
One of the reasons you might stop doing things you once enjoyed is a feeling of tiredness; low energy and fatigue are among the most debilitating symptoms of depression, which can lead to excessive sleepiness.
Depression is also linked with insomnia, as one might lead to the other and vice versa. They can also make each other worse. The lack of quality, restful sleep can also lead to anxiety.
Uncontrollable emotions
One minute it is an outburst of anger; the next, you are crying uncontrollably. Nothing outside of you prompted the change, but your emotions go up and down at a moment’s notice. Depression can cause mood swings. Crying spells can be a symptom of postpartum depression, which can occur in a woman after she has given birth.
Hopelessness
MDD is a mood disorder that affects the way you feel about life in general. Having a hopeless or helpless outlook on your life is the most common symptom of depression.
Other feelings may be worthlessness, self-hate, or inappropriate guilt. Common, recurring thoughts of depression are: “It’s all my fault,” or “What’s the point?”
Worthlessness
Persistent feelings of worthlessness, guilt, or helplessness are major symptoms in clinical depression. Depressed persons tend to focus on personal shortcomings or past failures. They often blame themselves when life is not going their way. Teenagers who experience depression; commonly report feelings of worthlessness; they may report feeling misunderstood and avoid interactions with others.
Sadness
The most common symptom of depression is a feeling of sadness or emptiness that lasts for more than two weeks. A person may describe this symptom as a feeling of “hopelessness.” They may feel as if life will not get better and that this intense level of sadness will last forever.
Lost interest
Depression can take the pleasure or enjoyment out of the things you love. A loss of interest or withdrawal from activities that you once looked forward to – sports, hobbies, or going out with friends – are telltale signs of depression.
Another area where you may lose interest in is sex. Symptoms of depression include a decreased sex drive and even impotence.
Fatigue
People with depression often experience a lack of energy or feel tired all the time. Small tasks, like showering or getting out of bed, may seem to need more effort than one can muster. Fatigue can play a role in other symptoms associated with depression, such as withdrawal and apathy. The person may feel overwhelmed at the mere thought of exertion or going outdoors.
Irritability
Depression may cause people to get frustrated or angered over insignificant matters. This often relates back to fatigue that makes it difficult to get through the day. Men and women may display irritability symptoms differently; women often report feeling angry at one moment, then tearful the next. Men may seem volatile.
Guilt
Depression is often the result of imbalanced chemicals in the brain. However, people experiencing depression may blame themselves for their symptoms instead. Statements such as “I can’t do anything right” or “everything is my fault,” become the person.
Anxiety
Experiencing occasional anxiety is a normal part of life; however, depression can cause a person to feel tense all the time without an identifiable source for the tension.
Depression has not been shown to cause anxiety, but the two conditions
often occur together. Symptoms of anxiety can include:
- Nervousness, restlessness, or feeling tense
- Feelings of danger, panic, or dread
- Rapid heart rate
- Rapid breathing
- Increased or heavy sweating
- Trembling or muscle twitching
- Trouble focusing or thinking clearly about anything other than the thing you are worried about
Restlessness
Agitation and restlessness, including pacing, an inability to sit still, or hand wringing, may occur with depression.
Lack of concentration
People with depression may have a difficult time remembering, maintaining focus, or making decisions. Fatigue, feelings of worthlessness, or feeling “numb” can turn decision-making into a task that is difficult to do. Friends or family members may discuss specific dates or events, but the person may not remember just moments later due to a lack of concentration. This inability to concentrate can lead to withdrawal in a depressed person.
Withdrawal
Many people with depression shut themselves off from the world. They may isolate themselves, not answer the phone, or refuse to go out with friends. They feel as if they are “numb” and that nothing will bring them joy.
Sleep problems

People’s sleep habits are likely to change because of depression. They may not be able to fall asleep or stay asleep. They may wake up in the middle of the night and not go back to sleep at all. You may sleep for long periods and find that you do not want to get out of bed. These symptoms lead to fatigue that can exacerbate more symptoms of depression, such as a lack of concentration.
Changes in appetite and weight
Depression can often cause a lack of interest in food and weight loss. In others, depression leads to overeating and weight gain. This is because a person may feel so frustrated or miserable that they turn to food to escape their problems; however, overeating can lead to weight gain and cause low levels of energy. Not enough food can also cause low energy levels and weakness.
Thoughts of suicide
The person who thinks or fantasizes about death needs immediate attention by skilled medical personnel. Thoughts of suicide are common symptoms in older men. Loved ones may not initially notice this thinking and pass a person’s depression symptoms off as age-related mental health changes. However, depression and especially suicidal thoughts are never normal emotions.
If you or a loved one is thinking of suicide, seek immediate medical attention at an emergency room, where a doctor can help you get mental health care until these feelings subside.
Physical pain
Physical symptoms, such as body pain, headaches, cramps, and digestive problems, can occur. Younger children with depression commonly report physical pain symptoms. They may refuse to go to school or cling to a parent due to the worry about their aches and pains.
Getting help
If you have had some of the previously mentioned symptoms for more than two weeks, you might be suffering from a major depressive disorder. Recognizing that you are depressed is essential to getting the right help.
Depression affects millions of people, but there are varying treatments available, from lifestyle changes to medications. No matter the path of treatment you choose, asking for professional help is the first step to getting back to feeling like yourself again.
Looking at death
People who die of suicide may have had symptoms that were missed or ignored. Often people will talk about it or make the first attempt before succeeding in ending their life. If you think someone is at immediate risk of self-harm or hurting another person:
- Call 911, your local emergency number, or 800-273-8255.
- Stay with the person until help arrives.
- Remove any guns, knives, medications, or other things that may cause harm.
- Listen, but do not judge, argue, threaten, or yell.
What causes depression?
There are several possible causes of depression. They can range from biological to circumstantial. Some people are more susceptible to depressive episodes, while others are not.
Genetic
Depression may be an inherited condition. You may have a higher likelihood of experiencing a depressive disorder at some point in your life if you have a family member with depression or another mood disorder. The exact genes involved are not known. Many genes may cause depression.
Early Childhood Trauma
Some events affect the way your body reacts to fear and stressful situations.
Familial, social, and environmental factors
Depression can be familial. Thus, thorough family history is important. Familial, social, and environmental factors seem to play a significant role in the course of depressive illness in children and youths, even in preschool children. René Spitz described anaclitic depression (marasmus) in infants being raised in an orphanage and in hospitalized children whose parents were not allowed to visit.
Brain Structure
There is a greater risk for depression if the frontal lobe of your brain is less active. However, scientists do not know if this happens before or after the onset of depressive symptoms.
Biochemical
Neurotransmitters in the brain — specifically serotonin, dopamine, or norepinephrine — affect feelings of happiness and pleasure and may be out of balance in people with depression. Antidepressants work to balance these neurotransmitters, mainly serotonin. How and why these neurotransmitters get out of balance and what role they play in depressive states is not fully understood.
Hormonal
Changes in hormone production or functioning could lead to the onset of depressive states. Any changes in hormone states — including menopause, childbirth, thyroid problems, or other disorders — could cause depression.
With postpartum depression, mothers develop symptoms of depression after giving birth. It is normal to be emotional because of the changing hormones, but postpartum depression is a serious condition.
Seasonal
If you have a major depressive disorder with a seasonal pattern, also known as a seasonal affective disorder, your mood is affected by seasonal changes. As daylight hours get shorter in the winter, many people develop feelings of lethargy, tiredness, and a loss of interest in everyday activities.
The condition occurs in up to 5-percent of the U.S. population each year. Seasonal depression is typically triggered by the onset of autumn and lasts throughout the winter, and it very rarely occurs in summer and spring.
Your doctor may prescribe medication or a lightbox to help treat this condition. The condition usually goes away once the days get longer.
Geography and distance from the equator play significant roles in this disorder. Women also represent 4 out of 5 people with the condition.
Situational
Losing a loved one or a job, financial troubles, or a sudden change in circumstances can have an impact on people and trigger depression.
Medical conditions
Certain conditions may put you at higher risk, such as chronic illness, insomnia, chronic pain, or attention-deficit hyperactivity disorder (ADHD).
Drug use
A history of drug or alcohol misuse can affect your risk. About 21 percent of people who have a substance use problem also experience depression.
In addition to the above causes, other risk factors for depression include:
- Low self-esteem or being self-critical
- Personal history of mental illness
- Certain medications
- Stressful events, such as loss of a loved one, economic problems, or a divorce
Many factors can influence feelings of depression, as well as who develops the condition and who does not.
However, in many cases, healthcare providers are unable to determine what is causing depression.
How does the initial presentation of depression vary in adults, children, and elderly persons?
Patients with depression may not initially present with a complaint of low mood, inability to feel pleasure, or other typical symptoms. In the primary care setting, where many of these patients first seek treatment, the presenting complaints often can be somatic (e.g., fatigue, headache, abdominal distress, or change in weight). Patients may complain of irritability or difficulty concentrating than about sadness or low mood.
Children with depression may present with misleading symptoms such as irritability, a decline in school performance, or social withdrawal. Elderly persons may present with confusion or a general decline in functioning; they also experience more somatic complaints, cognitive symptoms, and fewer complaints of sad or dysphoric mood.
A dysphoric mood state may be expressed by patients as sadness, heaviness, numbness, or sometimes irritability and mood swings. They often report a loss of interest or pleasure in their usual activities, difficulty concentrating, or loss of energy and motivation. Their thinking is often negative, frequently with feelings of worthlessness, hopelessness, or helplessness.
How is psychosis evaluated in depression?
Patients with a major depressive disorder commonly show ruminative thinking. (The process of continuously thinking about the same thoughts, which tend to be sad or dark, is called rumination. A habit of rumination can be dangerous to your mental health, as it can prolong or intensify depression as well as impair your ability to think and process emotions.) Nevertheless, it is important to evaluate each patient for evidence of psychotic symptoms because this affects initial management.
Psychosis, when it occurs in the context of unipolar depression, is usually congruent in its content with the patient’s mood state; for example, the patient may experience delusions of worthlessness or some progressive physical decline.
Which disorders are included in the differential diagnoses of suspected depression with symptoms of psychosis?
Symptoms of psychosis should prompt a careful history to rule out any of the following:
- Bipolar affective disorder
- Schizophrenia
- Schizoaffective disorder
- Substance abuse
- Organic brain syndrome
What is the basis for the diagnosis of depression?
No physical findings are specific to major depressive disorder; instead, the diagnosis is based on the history and the mental status examination. Nevertheless, a complete mental health evaluation should always include a medical evaluation to rule out organic conditions that might imitate a depressive disorder. Most of these falls into the following major general categories:
- Infection
- Medication
- Endocrine disorder
- Tumor
- Neurologic disorder
How might appearance and affect change in patients with major depression?
Most patients with major depressive disorder present with a normal appearance. In patients with more severe symptoms, a decline in grooming and hygiene, as well as a change in weight, may be present. Patients may show psychomotor retardation, which manifests as a slowing or loss of spontaneous movement and reactivity, as well as a flattening or loss of reactivity in the patient’s affect (i.e., emotional expression). Some patients with depression may manifest psychomotor agitation or restlessness.
How might speech change among persons with depression?
Speech may be normal, slow, monotonic, or lacking in spontaneity and content. A pressured speech should suggest anxiety or mania, whereas a disorganized speech should prompt an evaluation for psychosis. Racing thoughts could also be an indication of anxiety, mania, or hypomania.
What are the DSM-5 criteria for the diagnosis of depression?
The specific DSM-5 criteria for depression are outlined below.
At least 5 of the following symptoms had to have been present during the same 2-week period (and at least 1 of the symptoms must be diminished interest/pleasure or depressed mood):
- Depressed mood: For children and adolescents, this can also be an irritable mood
- Diminished interest or loss of pleasure in almost all activities (anhedonia)
- Significant weight change or appetite disturbance: For children, this can be failure to achieve expected weight gain
- Sleep disturbance (insomnia or hypersomnia)
- Psychomotor agitation or retardation
- Fatigue or loss of energy
- Feelings of worthlessness
- Diminished ability to think or concentrate, indecisiveness
- Recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or specific plan for committing suicide
The symptoms cause significant distress or impairment in social, occupational, or other important areas of functioning.
The symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition.
The disturbance is not better explained by a persistent schizoaffective disorder, schizophrenia, delusional disorder, or other specified or unspecified schizophrenia spectrum and other psychotic disorders
There has never been a manic episode or a hypomanic episode.
How are depressive disorders (clinical depression) rated in the DSM-5?
Depressive disorders can be rated as mild, moderate, or severe. The disorder can also occur with psychotic symptoms, which can be mood congruent or incongruent. Depressive disorders can be determined to be in full or partial remission.
Does bereavement induce depression?
DSM-5 notes the importance of distinguishing between normal sadness and grief from a major depressive disorder. While bereavement can induce great suffering, it does not typically induce a major depressive disorder. When the two exist concurrently, the symptoms and functional impairment are more severe, and the prognosis is worse compared to bereavement alone.
When a major depressive disorder is complicated by bereavement in persons with other vulnerabilities to depressive disorders, the diagnosis of a major depressive disorder requires clinical judgment based on the history and cultural context for expression of grief.
How is depression with anxious distress defined in the DSM-5?
Anxious distress is defined as the presence of at least 2 of the following symptoms:
- Feeling keyed up or tense
- Feeling unusually restless
- Difficulty concentrating because of worry
- Fear that something awful may happen
- Feeling of the potential loss of control
Severity is further specified as:
- Mild: Two symptoms
- Moderate: Three symptoms
- Moderate-severe: Four or five symptoms
- Severe: Four or five symptoms with motor agitation
High levels of anxiety are associated with higher suicide risk, longer duration of illness, and a greater likelihood of non-response to treatment.
How is depression with melancholic features defined in the DSM-5?
In depression with melancholic features, either a loss of pleasure in almost all activities or a lack of reactivity to usually pleasurable stimuli is present. Additionally, at least 3 of the following are required:
- A depressed mood that is distinctly different from the kind that is felt when a loved one is deceased
- Depression that is worse in the morning
- Waking up 2-hours earlier than usual
- Observable psychomotor retardation or agitation
- Significant weight loss or anorexia
- Excessive or inappropriate guilt
According to the DSM-5, when is depression with melancholic features applicable?
According to DSM-5, depression with melancholic features is applied only when there is a near-complete absence of the capacity for pleasure, not merely a diminution. A depressed mood that is more severe and longer-lasting, or present without a reason is not considered a distinct quality. Melancholic features are more frequent in in-patients and are less likely to occur in milder major depressive episodes. They are also more likely to be co-morbid with psychotic features.
What are the DSM-5 criteria for the diagnosis of depressive episodes with catatonia?
The DSM-5 criteria for the diagnosis of depressive episodes with catatonia need between 3 to 12 psychomotor features during most of the episodes:
- Stupor
- Catalepsy
- Waxy flexibility
- Mutism
- Negativism
- Posturing
- Mannerism
- Stereotypy
- Agitation, not influenced by external stimuli
- Grimacing
- Echolalia
- Echopraxia
What are the DSM-5 criteria for the diagnosis of atypical depression?
An episode of depression may have atypical features. Characteristics of this subtype are mood reactivity and exclusion of melancholic and catatonic subtypes in addition to 2 or more of the following at least 2-weeks:
- Increased appetite or significant weight gain
- Increased sleep
- Feelings of heaviness in arms or sensitivities of the legs that extend far beyond the mood disturbance episodes and result in significant impairment in social or occupational functioning
- A pattern of longstanding interpersonal rejection sensitivity that extends far beyond the mood disturbance episodes and results in significant impairment in social or occupational functioning
Which psychotic features may be present with major depressive disorder?
The presentation of severe major depressive disorder may include psychotic features. Psychotic features include delusions and hallucinations and are mood-congruent or mood incongruent. Mood-congruent psychoses are often consistent with classic depressive themes, such as personal inadequacy, guilt, disease, or deserved punishment. Mood incongruent psychoses are not consistent with these typical themes but may also occur in depression.
Major depressive disorder with psychotic features is considered a psychiatric emergency. Patients may require psychiatric hospitalization.
According to the DSM-5, which disorders have features of depression but do not meet the criteria for a specific depressive disorder?
The DSM-5 includes a class of disorders with features of depression that does not meet the criteria for a specific depressive disorder.
Examples include the following:
- Recurrent brief depression
- Short duration depressive episodes
- Depressive episodes with insufficient symptoms
Consult the DSM-5 for further details about the diagnostic criteria for other specified depressive disorders
What is the role of metabolic syndrome in major depressive disorder?
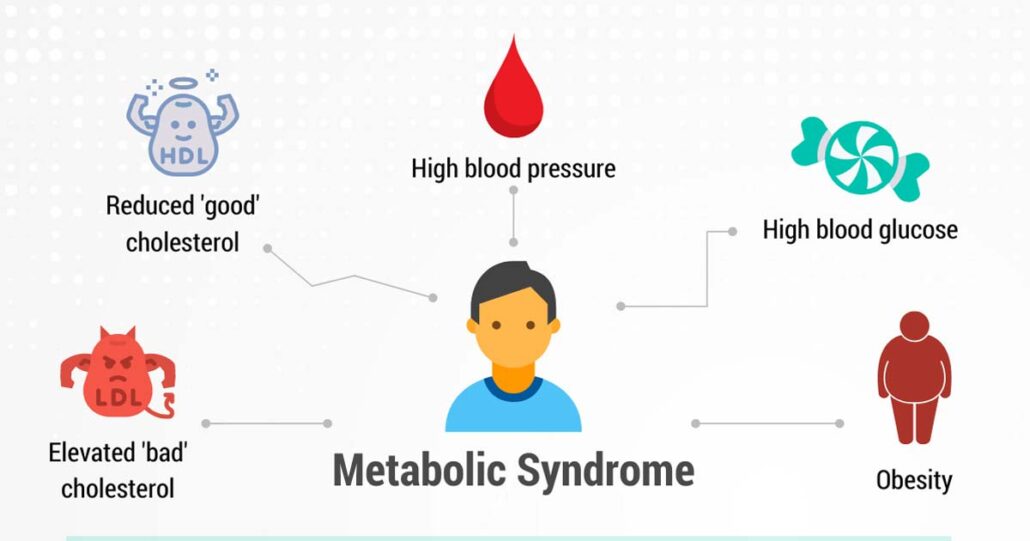
Several studies report an association between metabolic syndrome and depression. Vogelsong et al. suggest that later in life, waist circumference and not metabolic syndrome can predict the onset of depression. Specifically, the larger the waistline, the higher the incidence of depression. However, longitudinal studies have also shown that depression predicts subsequent obesity and centripetal obesity, likely because of poor diet, lack of exercise, and psychobiologic changes such as increased cortisol levels.
On the other hand, people with depression who have metabolic syndrome may simply be more likely to have persistent or recurrent depression. Thus, depression with metabolic abnormalities could be labeled metabolic depression, a possible chronic subtype of depression.
What is the role of cultural influences in the diagnosis of major depressive disorder?
Cultural influences on the presentation of depression can be significant. The practitioner should be aware of differences in the expression of psychological distress in patients from other countries or cultures.
Culturally distinctive experiences (e.g., fear of being hexed or bewitched; experience of visitations from the dead) should be distinguished from actual hallucinations or delusions that may be part of a major depressive episode with psychotic features.
When is assessment for suicidal ideation indicated in major depressive disorder?
Patients with depression should be assessed for suicidal ideation, especially if agitation is present. When a patient has contemplated or attempted suicide, the burden is on the health care provider to directly explore the situation with the patient in as much detail as possible to determine the current presence of suicidal ideation as well as accessible means and plans. Discussing these is the most important step clinicians can take to prevent suicide in an at-risk patient.
Which disorders should be included in the differential diagnoses of major depressive disorder?
The differential diagnosis for depression includes a wide variety of medical disorders, such as the following:
- Central nervous system diseases (e.g., Parkinson disease, dementia, multiple sclerosis, neoplastic lesions)
- Endocrine disorders (e.g., hyperthyroidism, hypothyroidism)
- Drug-related conditions (e.g., cocaine abuse, side effects of some CNS depressants)
- Infectious disease (e.g., mononucleosis)
- Sleep-related disorders
How is major depressive disorder differentiated from persistent depressive disorder?
Major depressive disorders must be differentiated from dysthymia. Patients with dysthymia present with low mood as a primary symptom for at least two years; they have insufficient symptoms to meet the criteria for major depressive disorder. However, dysthymia may predate a depressive episode.
How is major depressive disorder differentiated from bipolar disorder (manic depression)?
Misdiagnosis of bipolar disorder as recurrent unipolar depression may occur if the clinician does not identify the presence of hypomania between depressive episodes. This leads to inadequate treatment and, theoretically, to precipitation of a hypomanic, manic, or mixed episode.
Are anxiety disorders a risk factor for developing a major depressive disorder?
Patients with anxiety disorders are at a higher risk for developing co-morbid depression. In such patients, it is important to identify the anxiety disorder because affected individuals often require specific treatment approaches. Commonly encountered anxiety disorders include the following:
- Generalized anxiety disorder
- Obsessive-compulsive disorder
- Panic disorder
- Phobic disorders
- Posttraumatic stress disorder
How is major depressive disorder differentiated from personality disorders?
Patients with certain personality disorders (e.g., borderline personality disorder) may present with mood changes as a prominent symptom. Remember that the presence of a personality disorder can be difficult to determine in the setting of active affective symptoms. Many depressed patients who appear labile, demanding, or pathologically dependent look dramatically different once the depressive episode has been treated adequately.
Are eating disorders a risk factor for developing a major depressive disorder?
People with eating disorders also have a high rate of comorbid major depressive disorder and require specific treatment approaches. These disorders include bulimia, anorexia nervosa, and eating disorder not otherwise specified. A large percentage of individuals in this last group have binge-eating disorder.
Does major depressive disorder cause focal neurologic signs?
A major depressive disorder does not cause focal neurologic signs. Such findings should prompt an evaluation for other organic syndromes.
What is pseudodementia in patients with major depressive disorder?
A broad range of physiological and structural CNS processes can produce changes in mood and behavior. Note that a major depressive disorder can produce measurable cognitive deficits or a worsening of pre-existing dementia. This decline in cognitive functioning, which on formal testing appears to arise from impaired concentration or motivation, is referred to as pseudo-dementia or as dementia of depression and should remit with successful treatment of the depressive episode.
Alzheimer’s disease and other degenerative and vascular dementias can be associated with affective symptoms, especially in the initial phases of dementia. Mood disorders are also very prominent in Parkinson’s disease, Huntington’s disease, multiple sclerosis, stroke, and seizure disorders. Neoplastic lesions of the CNS can cause changes in mood and behavior before the onset of focal neurological signs.
Which endocrinologic disorders are likely to produce changes in mood?
Endocrinologic disorders involving the hypothalamic-pituitary-adrenal axis or thyroid are especially likely to produce changes in mood. These include Addison disease, Cushing syndrome, hyperthyroidism, hypothyroidism, prolactinomas, and hyperparathyroidism.
Which medications produce changes in mood?

Pharmacologic agents can produce changes in mood. These substances include the following:
- Antihypertensive medications (especially reserpine and methyldopa)
- Smoking-cessation aids (e.g., varenicline)
- Steroids
- Sex hormones and medications that affect sex hormones (e.g., estrogen, progesterone, testosterone, gonadotropin-releasing hormone [GnRH] antagonists)
- H2 blockers (e.g., ranitidine, cimetidine)
- Sedatives
- Muscle relaxants
- Appetite suppressants
- Chemotherapy agents (e.g., vincristine, procarbazine, L-asparaginase, interferon, vinblastine)
What is the role of antihypertensive agents in major depressive disorder?
Among antihypertensive agents, beta-blockers have a reputation for being strongly associated with depression. Research on this association has been somewhat contradictory, but suggests at most, a minor role in this regard. For example, a review by Ko et al. found no significant increased risk of depressive symptoms with beta-blockers, although there was a small but significant risk of fatigue and sexual dysfunction.
Risks appear to vary with different beta-blockers. A study by Luijendijk in elderly patients found that highly lipid-soluble beta-blockers (mostly propranolol) were associated with depressive symptoms during the first 3 months of use. In contrast, pindolol may accelerate or enhance the effects of antidepressant drugs.
Does calcium channel blockers (CCD) impair the effectiveness of antidepressants in the treatment of major depressive disorder?
Case reports have suggested a possible link between calcium channel blockers and depression. The principal concern with these agents, however, is that they may cause resistance to antidepressants.
What is the role of substance use in major depressive disorder?
Substance use, abuse, or dependence can cause significant mood symptoms. This is especially true of alcohol, cocaine, amphetamines, cannabinoids, sedatives/hypnotic, and narcotics. Inhalant abuse should also be considered, particularly among young male patients.
Which infectious processes can cause mood and behavior changes?
Infectious processes that can cause mood and behavior changes include Lyme disease, mononucleosis, human immunodeficiency virus (HIV) encephalopathy, and syphilis. Inflammatory conditions such as systemic lupus erythematosus (SLE), can produce a range of neuropsychiatric signs and symptoms. The likely mechanism in these cases is alterations in the blood-brain barrier and an autoimmune cerebritis.
Which sleep disorder can cause psychiatric symptoms?
Of the various sleep disorders, obstructive sleep apnea can cause significant medical and psychiatric symptoms and is often missed as a diagnosis. Patients and, if necessary, their partners should be interviewed regarding their sleep quality, daytime sleepiness, and snoring. Obstructive sleep apnea is especially common in patients with obesity. Polysomnography can help make the diagnosis and guide treatment.
What are the differential diagnoses for Depression?
- Adjustment Disorders
- Anemia
- Chronic Fatigue Syndrome
- Dissociative Disorders
- Hypochondriasis
- Hypoglycemia
- Hypopituitarism (Panhypopituitarism)
- Schizoaffective Disorder
- Schizophrenia
- Somatic Symptom Disorders
What is a common complaint of patients with major depressive disorder?
Patients with major depressive disorder often complain of poor memory or concentration. This may be due to the depression itself or to an underlying dementia.
Which lab tests are useful to exclude medical illnesses that may present as a major depressive disorder?
Depression is a clinical diagnosis based on history and physical findings.
No laboratory tests are available to diagnose a major depressive disorder, but focused laboratory studies may be useful to exclude potential medical illnesses that may present as major depressive disorders. These laboratory studies might include the following:
- Complete blood cell (CBC) count
- Thyroid-stimulating hormone (TSH)
- Vitamin B-12
- Rapid plasma reagin (RPR)
- HIV test
- Electrolytes, including calcium, phosphate, and magnesium levels
- Blood urea nitrogen (BUN) and creatinine
- Liver function tests (LFTs)
- Blood alcohol level
- Blood and urine toxicology screen
- Arterial blood gas (ABG)
- Dexamethasone suppression test (Cushing disease, but also positive in depression)
- Cosyntropin (ACTH) stimulation test (Addison disease)
Psychosis
Patients with a major depressive disorder commonly show ruminative thinking. (The process of continuously thinking about the same thoughts, which tend to be sad or dark, is called rumination. A habit of rumination can be dangerous to your mental health, as it can prolong or intensify depression as well as impair your ability to think and process emotions). Nevertheless, it is important to evaluate each patient for evidence of psychotic symptoms because this affects initial management.
Psychosis, when it occurs in the context of unipolar depression, is usually congruent in its content with the patient’s mood state. The patient may experience delusions of worthlessness or some progressive physical decline.
Symptoms of psychosis should prompt a careful history and evaluation to rule out any of the following:
- Bipolar affective disorder
- Schizophrenia
- Schizoaffective disorder
- Substance abuse
- Organic brain syndrome
Do antidepressants increase or decrease suicidal behavior in patients with major depressive disorder?
Antidepressants were associated with a significant reduction in the risk of suicidal behavior in an observational study by Leon et al., which followed 757 patients over a 27-year period. This study included participants with psychiatric and other medical disorders and those receiving acute or maintenance therapy, polypharmacy, or no psychopharmacologic treatment at all. The results suggest, however, that clinicians must closely monitor patients when an antidepressant is prescribed.
Other studies have argued that a decline in youth suicide rates coincided, to a striking extent, with significant increases in the prescription of antidepressants (mostly SSRIs) to adolescents. The Treatment for Adolescents with Depression Study (TADS) lends support for fluoxetine’s efficacy in adolescent depression, notably the combined use of fluoxetine and CBT. Data from the TADS study also suggested a possible protective effect of CBT against suicidality when used in combination with fluoxetine.
A study by the Group Health Cooperative in Seattle of more than 65,000 children and adults treated for depression found that suicide risk declines, not rises, with the use of antidepressants. This is the largest study to date to discuss this issue. This study also showed that with psychotherapy and antidepressant drug therapy, the highest risk of suicide was in the month before seeking treatment. The month following initiation of treatment was also a period of high risk for both types of treatment, emphasizing close follow-up after treatment initiation.
When are tricyclic antidepressants (TCAs) indicated in the treatment of children with major depressive disorder?
TCAs are no longer considered the first-line treatment for pediatric patients with depressive disorders; however, individual cases may respond better to TCAs than to other medications. TCAs may also be useful for those with comorbid attention deficit hyperactivity disorder (ADHD), enuresis, and narcolepsy, as well as for augmentation strategies.
Which baseline and monitoring tests are required when tricyclic antidepressants are administered for the treatment of major depressive disorder?
The TCAs require a baseline electrocardiogram (ECG), resting blood pressure, and pulse rate. Because of the potential of the TCAs to induce a fatal overdose, the clinician must carefully determine the exact amount of medication to be prescribed. Plasma levels should be monitored to measure compliance and to avoid toxicity. In addition, weight should be frequently documented.
No laboratory tests are currently indicated before or during the administration of the SSRIs. No other tests are indicated in a healthy child before starting antidepressants.
Are effective treatments available for major depressive disorder?
A wide range of effective treatments is available for major depressive disorder. Medication alone and brief psychotherapy (e.g., cognitive-behavioral therapy, interpersonal therapy) alone can relieve depressive symptoms. There is also empirical support for the ability of brief psychotherapy (CBT) to prevent relapse.
In children and adolescents, however, pharmacotherapy by itself is insufficient treatment. Moreover, in all patient populations, the combination of medication and psychotherapy generally provides the quickest and most sustained response. Combination therapy has also been associated with higher rates of improvement in depressive symptoms: increased quality of life; better treatment compliance, especially when treatment is needed for longer than 3-months.
What factors should be considered in medication selection for the treatment of major depressive disorder?
Usually, 2–12 weeks at therapeutic dosage with the adherence to the regimen is needed for a clinical response. The choice of medication should be guided by safety and tolerability, which aid in compliance; physician familiarity, which aids in patient education and anticipation of adverse effects; and history of previous treatments. Often, treatment failures are caused by medication non-compliance, inadequate duration of therapy, or inadequate dosing.
What are the ACP guidelines for the use of second-generation anti-depressants in the treatment of major depressive disorder?

According to the 2008 American College of Physicians (ACP) guideline on second-generation antidepressants, patient preferences should be given serious consideration when choosing pharmacotherapy for depressive disorders. A patient may want to avoid the use of an antidepressant if he or she had previous negative experience with the drug.
What are the ACP guidelines for the duration of pharmacotherapy in major depressive disorder?
The 2008 ACP guideline recommends that the treatment for major depressive disorder should be altered if the patient does not have an adequate response to pharmacotherapy within 6–8 weeks. Once a satisfactory response is achieved, the treatment should be continued for 4–9 months in patients with the first episode of major depression that was not associated with significant suicidality or catastrophic outcomes. In those who have had 2 or more episodes of depression, a longer course of maintenance treatment may prove beneficial.
What are the APA guidelines for treatment selection for major depressive disorder?
In 2011, the American Psychiatric Association (APA) updated its Practice Guideline for the Treatment of Patients with Major Depressive Disorder. The 2011 APA guideline emphasizes the need to customize a treatment plan for each patient based on a careful assessment of symptoms, including rating scale measurements administered by a clinician or the patient, as well as an analysis of therapeutic benefits and side effects.
Treatment should maximize patient function within specific and realistic goals. The initial modality should be chosen based on the following:
- Clinical assessment
- Presence of other disorders
- Stressors
- Patient preference
- Reactions to previous treatment
How often is psychotherapy conducted in the treatment of major depressive disorder?
Psychotherapy is often conducted on an outpatient basis with weekly, 60-minute sessions. Although there is wide variation in practice, psychotherapy tends to be time-limited (e.g.,16 sessions).
According to the APA guidelines, when are psychological treatments considered efficacious?
In the 1990s, the American Psychological Association’s Division 12 Task Force on Promotion and Dissemination of Psychological Procedures developed criteria for evaluating the empirical support for psychological treatments. Chambless and Hollon refined these guidelines such that a therapy is considered efficacious and specific if there is evidence from high-quality studies in two or more settings indicating that it is superior to a pill or psychological placebo or to another bona fide treatment. A treatment is considered efficacious if there is evidence from two or more settings that it is superior to no treatment. A therapy is possibly efficacious if there is research support from one or more studies in a single setting. It is recommended that individuals seeking psychotherapy for depression receive one with empirical support.
What drugs are used for the treatment of major depressive disorder?
Drugs used for the treatment of depression include the following:
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin/norepinephrine reuptake inhibitors (SNRIs)
- Atypical antidepressants
- Serotonin-Dopamine Activity Modulators (SDAMs)
- Tricyclic antidepressants (TCAs)
- Monoamine oxidase inhibitors (MAOIs)
- N-methyl-D-aspartate (NMDA) receptor antagonists
- St. John’s wort
Is St. John’s Wort effective in the treatment of major depressive disorder?
St. John’s Wort (Hypericum perforatum) is an herbal remedy available over the counter. Although St. John’s Wort is considered a first-line antidepressant in many European countries, it has only recently gained popularity in the United States. Uses include treatment of mild to moderate depressive symptoms. It is not effective in major depressive episodes.
St. John’s Wort may act as an SSRI. The usual dosage is 300 mg 3 times a day with meals to prevent GI upset. If no clinical response occurs after 3–6 months, the use of another medication is recommended.
In addressing the issue of alternative therapies for depression, the 2011 APA guideline noted that St. John’s Wort might be considered, but evidence for its effectiveness is modest, and more information is needed about its interaction with other drugs.
Which SSRIs are used in the treatment of major depressive disorder?
SSRIs include the following:
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
- Fluvoxamine (Luvox)
- Paroxetine (Paxil)
- Sertraline (Zoloft)
- Vilazodone (Viibryd)
- Vortioxetine (Brintellix)
What are the advantages of SSRIs for the treatment of major depressive disorder?
SSRIs have the advantage of the ease of dosing and low toxicity in an overdose. SSRIs are preferred over the other classes of antidepressants for the treatment of children and adolescents and are the first-line medications for late-onset depression. The 2011 APA guideline supports this recommendation.
What are the possible adverse effects of SSRIs in the treatment of major depressive disorder?
The adverse-effect profile of SSRIs is less prominent than that of some other agents, which promotes better compliance. Common adverse effects include gastrointestinal upset, sexual dysfunction, and changes in energy level (i.e., fatigue, restlessness).
Are SSRIs contraindicated in patients with comorbid major depressive disorder and cardiac disease?
The SSRIs are relatively safe in patients with cardiac disease, as these agents do not seem to affect blood pressure, heart rate, cardiac conduction, or cardiac rhythm. However, citalopram can cause dose-dependent QT prolongation.
When is citalopram contraindicated in the treatment of major depressive disorder?
The US Food and Drug Administration (FDA) does not recommend citalopram in patients with congenital long QT syndrome. Citalopram may be used for patients with this condition who lack viable alternatives; however, it should be given at a low dose, with EKG and electrolyte monitoring. Citalopram should be discontinued in patients who are found to have a persistent corrected QT interval greater than 500 ms.
The dose of citalopram should not exceed 40 mg/day because of the risk of potentially fatal cardiac arrhythmias; furthermore, higher doses have not been shown more effective in treating depression. For patients older than 60 years, the maximum recommended dose of citalopram is 20 mg/day.
Is vortioxetine (Brintellix) effective in the treatment of major depressive disorder?
In September 2013, the FDA approved vortioxetine (Brintellix) for major depressive disorder in adults. The drug’s mechanism of action involves the enhancement of serotonergic activity through 5-HT reuptake inhibition. It also modulates serotonin receptor activity through 5-HT1A receptor agonism and 5-HT3 receptor antagonism, although the contribution of these activities to the antidepressant effect is not fully understood.
Approval was based on 5 short-term (6-8 week) studies, including one that focused on elderly adults. These studies demonstrated a statistically significant reduction in overall symptoms of depression with vortioxetine compared to placebo, with the most consistent results obtained within a dosage range of 15-20 mg/day. Also, a long-term (24-64 week) maintenance study showed a longer time to relapse with vortioxetine compared to placebo. Two studies using lower doses (2.5-5 mg/day) showed no significant difference in efficacy between the drug and placebo. The most common adverse effects were nausea, diarrhea, dry mouth, constipation, vomiting, dizziness, and sexual dysfunction.
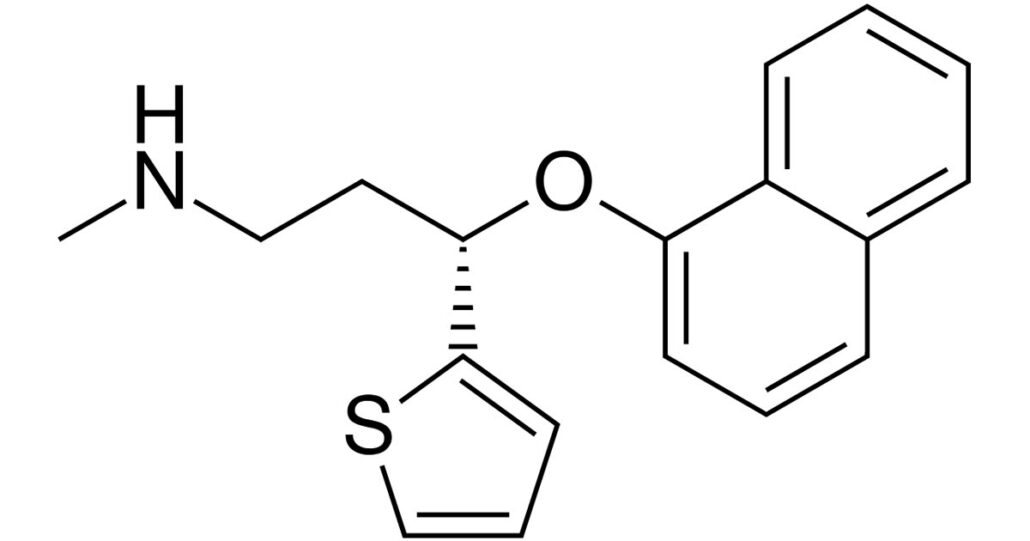
What is the role of SNRIs in the treatment of major depressive disorder?
SNRIs, which include venlafaxine (Effexor); desvenlafaxine (Pristiq); duloxetine (Cymbalta); and levomilnacipran (Fetzima); can be used as first-line agents, particularly in patients with significant fatigue or pain syndromes associated with depression. SNRIs also have an important role as second-line agents in patients who have not responded to SSRIs.
Is concurrent use of SNRIs with other antidepressants safe and effective in the treatment of major depressive disorder?
The concurrent use of SNRIs with other antidepressants may be more problematic. For example, the Combining Medications to Enhance Depression Outcomes (CO-MED) study found that the combination of extended-release venlafaxine plus mirtazapine may pose a greater risk of adverse events and does not outperform monotherapy.
The safety, tolerability, and side-effect profiles of SNRIs include those of the SSRIs, as well as noradrenergic side effects, such as hypertension.
Is levomilnacipran (Fetzima) effective in the treatment of major depressive disorder?
In July 2013, the FDA approved the newest SNRI, levomilnacipram (Fetzima), which is available as a once-daily sustained-release formulation. It has greater potency for norepinephrine reuptake inhibition than for serotonin reuptake inhibition without directly affecting the uptake of dopamine or other neurotransmitters.
Which atypical antidepressants are effective in major depressive disorder?
Atypical antidepressants include bupropion (Wellbutrin), mirtazapine (Remeron), nefazodone, and trazodone (Desyrel). They have all been found to be effective in monotherapy in major depressive disorder and may be used in combination therapy for more difficult to treat depression.
Nevertheless, this group also shows low toxicity in overdose.In addition, bupropion has the advantage over SSRIs of causing less sexual dysfunction and GI distress. Mirtazapine is associated with a high risk of weight gain, so patients who are treated with this agent should have a careful monitoring of weight.
What is the role of SDAMs in the treatment of major depressive disorder?
SDAMs include brexpiprazole (Rexulti) and aripiprazole (Abilify). SDAMs act as a partial agonist at 5-HT1A and dopamine D2 receptors at similar potency, and as an antagonist at 5-HT2A and noradrenaline alpha1B/2C receptors. This mechanism of action is unique from other atypical antipsychotic drugs.
Brexpiprazole is indicated as adjunctive therapy for major depressive disorder (MDD). Aripiprazole is indicated for schizophrenia, acute treatment of manic and mixed episodes associated with bipolar I, as an adjunct to MDD, irritability associated with autistic disorder, and treatment of Tourette disorder. Also, aripiprazole prompt-acting injection is indicated for agitation associated with schizophrenia or bipolar mania.
Are SDAMs effective in the treatment of major depressive disorder?
In clinical trials, brexpiprazole was added to existing antidepressant therapy in patients who had failed multiple trials of antidepressant therapy. Patients enrolled met DSM-IV-TR criteria for MDD. Brexpiprazole (2-mg and 3-mg daily) plus antidepressant therapy was superior to placebo plus antidepressant therapy on the primary endpoint (i.e., change in Montgomery-Åsberg Depression Rating Scale scores).
Which tricyclic antidepressants (TCAs) are effective in major depressive disorder?
TCAs include the following:
- Amitriptyline (Elavil)
- Clomipramine (Anafranil)
- Desipramine (Norpramin)
- Doxepin (Sinequan)
- Imipramine (Tofranil)
- Nortriptyline (Pamelor)
- Protriptyline (Vivactil)
- Trimipramine (Surmontil)
TCAs have a long record of efficacy in the treatment of depression. They are used less commonly because of their side-effect profile and their considerable toxicity in overdose.
Are MAOIs effective in the treatment of major depressive disorder?
MAOIs include isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Emsam), and tranylcypromine (Parnate). These agents are widely effective in a broad range of affective and anxiety disorders. Because of the risk of hypertensive crisis, patients on these medications must follow a low-tyramine diet. Other adverse effects can include insomnia, anxiety, orthostasis, weight gain, and sexual dysfunction.
Is psilocybin effective in the treatment of major depressive disorder?
Psilocybin, a classic “psychedelic” drug, along with psychological support, is showing promise as a treatment for patients with treatment-resistant depression. A study of 19-patients measured cerebral blood flow (CBF) and blood oxygen-level dependent (BOLD) resting-state functional connectivity (RSFC) with functional magnetic resonance imaging (fMRI) before and after treatment with psilocybin. All 19-patients exhibited decreased depressive symptoms one-week post-treatment, and 47% met the criteria for response at 5-weeks. Whole-brain analyses revealed post-treatment decreases in CBF in the temporal cortex, including the amygdala. Decreased amygdala CBF correlated with reduced depressive symptoms.
The Agency for Healthcare Research and Quality (AHRQ) compared the effectiveness of the following 12 second-generation antidepressants:
- Bupropion
- Citalopram
- Duloxetine
- Escitalopram
- Fluoxetine
- Fluvoxamine
- Mirtazapine
- Paroxetine
- Sertraline
- Trazodone
- Venlafaxine
The AHRQ found that the average effectiveness of the antidepressants appeared similar, but the studies reviewed were not designed to test the variations among patients’ responses. However, the AHRQ did find moderately strong evidence of differences among second-generation antidepressants with respect to the onset of action and measures (e.g., sexual functioning) that could affect health-related quality of life.
What are the ACP guidelines for the selection of second-generation antidepressants in the treatment of major depressive disorder?
The 2008 ACP guideline advises clinicians to choose second-generation antidepressants based on adverse effects, cost, and patient preferences since all these agents have comparable efficacy.
Which treatments are effective in major depressive disorder with suicidal ideation?

Zisook et al. found that among depressed patients with suicidal ideation at baseline, sustained-release bupropion and escitalopram were more effective at reducing suicidal ideation than sustained-release venlafaxine plus mirtazapine; the former was most effective at week 12 of treatment. In this study, of 665 outpatients with non-psychotic chronic and/or recurrent major depressive disorder, 4-patients attempted suicide; all were receiving venlafaxine plus mirtazapine.
Does the effectiveness of antidepressant medications increase with depression severity?
In a meta-analysis, Fournier et al. found that medication superiority over placebo increased with increases in baseline depression severity, crossing the threshold for a clinically significant difference at a baseline Hamilton Depression Rating Scale (HDRS) score of 25.
In patients with mild to moderate depression, antidepressant medications had minimal or no benefits compared with a placebo. In patients with very severe depression, antidepressant drugs provided a substantial benefit compared with placebo.
More confirmation that antidepressants work for depression came from a large meta-analysis of 522 randomized controlled trials that compared 21 different antidepressants with placebo in more than 116,000 patients with major depressive disorder.
The 21 antidepressants included in the trials were: agomelatine; amitriptyline; bupropion; citalopram; clomipramine; desvenlafaxine; duloxetine; escitalopram; fluoxetine; fluvoxamine; levomilnacipran; milnacipran; mirtazapine; nefazodone; paroxetine; reboxetine; sertraline; trazodone; venlafaxine; vilazodone; and vortioxetine. Results showed that each studied antidepressant was more efficacious, defined as yielding a reduction of at least 50% in the total score of a standardized scale for depression than placebo after 8-weeks. Patients who received agomelatine, escitalopram, and vortioxetine had both high response rates and low dropout rates.
Antidepressants, SSRIs
Class Summary
SSRIs are the initial antidepressants of choice for uncomplicated depression because of their minimal anticholinergic side effects, such as dry mouth, constipation, urinary retention, bowel obstruction, dilated pupils, blurred vision, increased heart rate, and decreased sweating.
They have the advantage of ease of dosing and low toxicity in overdose. SSRIs are greatly preferred over the other classes of antidepressants for the treatment of children and adolescents, and these agents are also the first-line medications for late-onset depression, due to their superior tolerability and comparatively more benign safety profile.
The SSRIs are not thought to be as worrisome in patients with cardiac disease, as they do not appear to exert any effect on blood pressure, heart rate, cardiac conduction, or cardiac rhythm; however, dose-dependent QT prolongation has been reported with citalopram. Because of the risk for QT prolongation, citalopram is contraindicated in individuals with congenital long QT syndrome.
Because the adverse-effect profile of SSRIs is less prominent than other agents, improved compliance is promoted. Common adverse effects of SSRIs include gastrointestinal upset, sexual dysfunction, bleeding, emotional blunting, cognitive dysfunction, and changes in energy level (i.e., fatigue, restlessness).
The US Food and Drug Administration issued a safety information update in December 2011 concluding that it is unclear whether the use of SSRIs during pregnancy causes persistent pulmonary hypertension in the newborn. The FDA currently recommends that health care professionals and patients weigh the small potential risk of persistent pulmonary hypertension against the substantial risks of untreated depression during pregnancy.
Citalopram (Celexa)
Citalopram enhances serotonin activity because of selective reuptake inhibition at the presynaptic neuronal membrane. It has minimal effects on norepinephrine and dopamine.
Although it has FDA approval only for depression, citalopram is commonly prescribed for other psychiatric disorders, including obsessive-compulsive disorder, generalized anxiety disorder, panic disorder, and premenstrual dysphoric disorder.
The FDA advises that the dose of citalopram not exceed 40 mg/day because of the risk of potentially fatal QT prolongation. Furthermore, higher doses have not been shown to be more effective in treating depression.
Escitalopram (Lexapro)
Escitalopram is an SSRI and S-enantiomer of citalopram used for the treatment of depression. The mechanism of action is thought to be the potentiation of serotonergic activity in the central nervous system resulting from inhibition of CNS neuronal reuptake of serotonin. Escitalopram has little or no effect on norepinephrine and dopamine reuptake.
Onset of depression relief may occur after 1-2 week, but individual responses vary, and a full effect may not be seen until 8-12 weeks.
Fluoxetine (Prozac)
Fluoxetine is a commonly used SSRI and was the first of the SSRIs to become available in the United States. It selectively inhibits presynaptic serotonin reuptake with minimal or no effect on the reuptake of norepinephrine or dopamine. It is commonly prescribed for many indications that are not FDA approved, including fibromyalgia, posttraumatic stress disorder, Raynaud phenomenon, social anxiety disorder, and selective mutism.
Fluvoxamine
Fluvoxamine enhances serotonin activity due to selective reuptake inhibition at the neuronal membrane. It does not significantly bind to alpha-adrenergic, histamine, or cholinergic receptors and thus has fewer side effects than tricyclic antidepressants. Fluvoxamine is a strong inhibitor of cytochrome P-450. Although fluvoxamine is FDA approved only for obsessive-compulsive disorder, it is commonly prescribed for other psychiatric disorders, including social anxiety disorder, posttraumatic stress disorder, pain disorder, and major depression.
Paroxetine (Paxil, Pexeva)
Paroxetine is a potent selective inhibitor of neuronal serotonin reuptake and has a weak effect on norepinephrine and dopamine neuronal reuptake. It has slight anticholinergic effects and may cause more weight gain than other SSRIs. Paroxetine is sometimes prescribed for indications that are not FDA approved, such as eating disorders and the relief of vasomotor symptoms of menopause.
Sertraline (Zoloft)
Sertraline selectively inhibits presynaptic serotonin reuptake. It has very minimal effects on norepinephrine and dopamine neuronal uptake. Sertraline is sometimes prescribed for indications that are not FDA approved, such as eating disorders, generalized anxiety disorder, and panic disorder.
Vilazodone (Viibryd)
Vilazodone’s mechanism of antidepressant effect is related to serotonergic activity in the CNS through selective inhibition of serotonin reuptake. This agent is also a partial agonist at serotonergic 5-HT1A receptors, although the contribution of this activity to the drug’s antidepressant effect is unknown.
Vilazodone is indicated for major depressive disorder. The dose should be adjusted when this agent is given with moderate or strong CYP3A4 inhibitors.
Vortioxetine (Trintellix)
Enhances serotonergic activity through 5-HT reuptake inhibition. It also modulates serotonin receptor activity through 5-HT1A receptor agonism and 5-HT3 receptor antagonism, although the contribution of these activities to the antidepressant effect is not fully understood. It is approved to treat the major depressive disorder in adults.
Antidepressants, SNRIs
Class Summary
SNRIs can be used as first-line agents, particularly in patients with significant fatigue or pain syndromes associated with the episode of depression. The SNRIs also have an important role as second-line agents in patients who have not responded to SSRIs. Safety, tolerability, and side-effect profiles are like those of the SSRIs, with the exception that venlafaxine and desvenlafaxine have been associated (rarely) with a sustained rise in blood pressure. Venlafaxine has been particularly associated with hyponatremia.
Desvenlafaxine (Pristiq, Khedezla)
Desvenlafaxine is an SNRI that is indicated for the treatment of the major depressive disorder.
Duloxetine (Cymbalta, Drizalma Sprinkle)
Duloxetine is a potent inhibitor of neuronal serotonin and norepinephrine uptake, and antidepressant action is thought to be due to serotonergic and noradrenergic potentiation in the central nervous system.
Venlafaxine (Effexor XR)
Venlafaxine and its active metabolite inhibit neuronal serotonin and norepinephrine reuptake. They are weak inhibitors of dopamine reuptake. In addition, it causes beta-receptor down-regulation. Venlafaxine is sometimes prescribed for non–FDA-approved indications, such as obsessive-compulsive disorder, hot flashes, neuropathic pain, attention-deficit/hyperactivity disorder, and posttraumatic stress disorder.
Levomilnacipran (Fetzima)
Levomilnacipran is the active enantiomer milnacipran and should be administered once daily. It is a potent inhibitor of neuronal serotonin and norepinephrine reuptake and inhibits norepinephrine uptake with approximately 3-fold higher potency in vitro than serotonin without directly affecting the uptake of dopamine or other neurotransmitters.
Antidepressants, TCAs
Class Summary
TCAs have a long record of efficacy in the treatment of depression and have the advantage of lower cost. They are used less commonly because of the need to titrate the dose to a therapeutic level and because of their considerable toxicity in overdose. TCAs are often prescribed for many other psychiatric disorders, such as generalized anxiety disorder and posttraumatic stress disorder. They are also used to treat chronic pain, such as neuropathy, and migraine headaches.
Amitriptyline (Elavil)
Amitriptyline inhibits the reuptake of norepinephrine and, more potently, serotonin at the presynaptic neuronal membrane, which increases the concentration in the CNS. It has a high affinity for histamine H1 and muscarinic M1 receptors. Amitriptyline can cause weight gain, sedation, and anticholinergic side effects. It is often used for non–FDA-approved indications, such as chronic pain management, diabetic neuropathy, migraine prophylaxis, and posttraumatic stress disorder.
Desipramine (Norpramin)
Desipramine inhibits the reuptake of serotonin and, more potently, norepinephrine at the presynaptic neuronal membrane. It is a commonly used TCA that is relatively less sedating and tends to have fewer anticholinergic and antihistaminic adverse effects than other TCAs. It is sometimes used for off-label indications such as peripheral neuropathy and attention-deficit/hyperactivity disorder.
Imipramine (Tofranil)
Imipramine is one of the oldest agents available for the treatment of depression. It is demethylated in the liver to desipramine. Imipramine inhibits the reuptake of norepinephrine and, more potently, serotonin at the presynaptic neuronal membrane. It has a strong affinity for alpha-adrenergic, H1, and M1 receptors. Common side effects include orthostasis, sedation, weight gain, and anticholinergic effects. It is also used off-label in the treatment of the panic disorder, posttraumatic stress disorder, and attention deficit/hyperactivity disorder.
Clomipramine (Anafranil)
Clomipramine potently inhibits the reuptake of serotonin at the presynaptic neuronal membrane. It has strong affinities to both H1 and M1 receptors, which results in sedation, weight gain, and anticholinergic side effects. Although clomipramine is FDA approved only for obsessive-compulsive disorder, it has also been prescribed for depression, panic attacks, and chronic pain.
Nortriptyline (Pamelor)
Nortriptyline blocks the reuptake of serotonin and, more potently, norepinephrine at the presynaptic neuronal membrane. It has less affinity for H1 and M1 receptors and, thus, is better tolerated than other TCAs. Although nortriptyline is FDA approved only for depression, it has also been prescribed for chronic pain, myofascial pain, anxiety disorders, and attention-deficit/hyperactivity disorder. As with desipramine, there is a therapeutic window for nortriptyline
Protriptyline
Protriptyline increases the synaptic concentration of norepinephrine in the CNS by inhibiting reuptake at the presynaptic neuronal membrane. It has less affinity for H1 and M1 receptors and, thus, is better tolerated than tertiary amine TCAs.
Doxepin
Doxepin increases the concentration of serotonin and norepinephrine in the CNS by inhibiting their reuptake at the presynaptic neuronal membrane. These effects are associated with a decrease in the symptoms of depression. It has the highest affinity for H1 receptors of all TCAs and, thus, is very sedating and can cause weight gain.
Trimipramine (Surmontil)
Trimipramine inhibits the reuptake of norepinephrine and serotonin at the presynaptic neuron and elicits strong anticholinergic effects. It has a high affinity for the H1 receptor and is thus very sedating, but it is useful for gastroesophageal reflux.
Amoxapine
Amoxapine inhibits the reuptake of norepinephrine and, to a lesser extent, serotonin at the presynaptic neuron. It also blocks dopamine receptors, causing it to have antipsychotic activity, as well.
What are the possible adverse effects of SSRIs in the treatment of major depressive disorder?, MAO Inhibitors
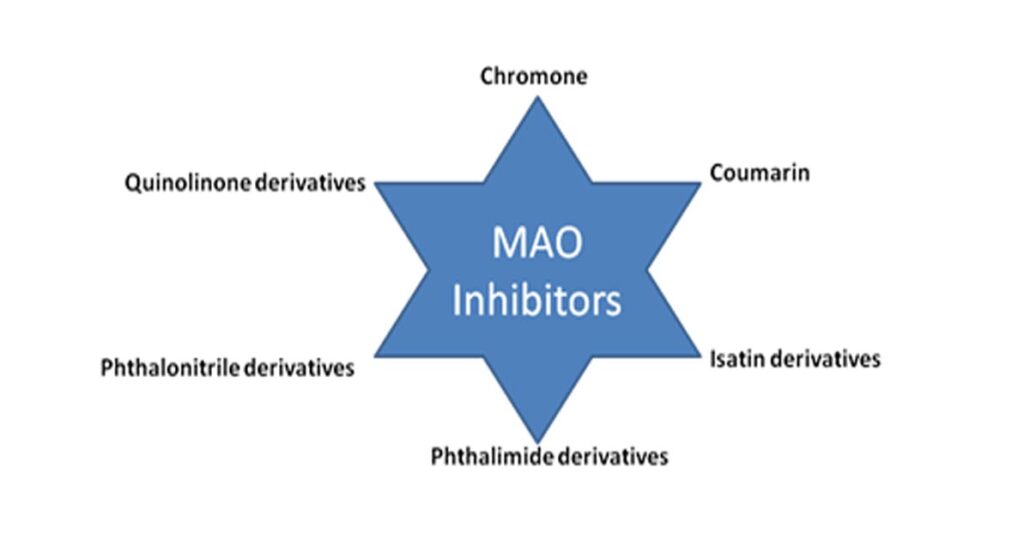
Class Summary
Monoamine oxidase inhibitors were the first antidepressants discovered, in the early 1950s. They are widely effective in a broad range of affective and anxiety disorders. MAOIs irreversibly block monoamine oxidase, which has 2 forms, including MOAa and MOAb. MAOa breaks down serotonin and norepinephrine. MOAb metabolizes phenylethylamine. Both forms break down dopamine.
MOAIs are not considered first-line treatment for depression because of the side effects, drug-drug interactions, and dietary restrictions. Common side effects include hypotension, dizziness, dry mouth, gastrointestinal upset, urinary hesitancy, headache, and myoclonic jerks. Because of the risk of hypertensive crisis with drugs that specifically inhibit MAOa in the gastrointestinal tract, patients on these medications must follow a low-tyramine diet.
Selegiline transdermal patch (Emsam)
Selegiline inhibits MAOb at lower doses and both forms at higher doses. Because it does not inhibit MAOa, it does not require dietary restrictions at lower doses. Lower doses of oral selegiline (Eldepryl) appear to lack antidepressant properties and are usually prescribed to treat Parkinson’s disease. Higher doses are used to treat the major depressive disorder, and the selegiline transdermal patch is FDA approved for this indication. Selegiline is sometimes used off-label to treat attention-deficit/hyperactivity disorder.
Dietary restrictions are not required for the 6 mg/24-hour patches because there is no risk of hypertensive crisis with this dose, given the lack of MAOa inhibition. Higher doses require dietary restrictions. The patch may be beneficial to those that cannot take oral medications. To avoid serotonin syndrome, initiating and stopping selegiline must be handled carefully.
Tranylcypromine (Parnate)
Tranylcypromine is used to treat major depression. It binds irreversibly to MAOa and to a lesser extent to MAOb, thereby reducing monoamine breakdown and enhancing synaptic availability. Clinical effects are not normally seen for 2-4 weeks. It has similar side effects as other MAOIs, but it is more likely to cause insomnia.
Phenelzine (Nardil)
Phenelzine is used to treat depression. It irreversibly inhibits both MOAa and MOAb. Side effects are like those of other MAOIs, but anticholinergic side effects are more common. Phenelzine causes less insomnia than tranylcypromine but is more likely to cause sedation, weight gain, and sexual dysfunction.
Isocarboxazid (Marplan)
Isocarboxazid is a nonselective hydrazine MAOI that is indicated for the treatment of depression. The mechanism by which MAOIs act as an antidepressant is not fully understood, but it is thought to be that these drugs increase the CNS concentrations of norepinephrine, dopamine, and serotonin.
Augmenting Agents
Class Summary
Augmentation is a common strategy for treatment-resistant depression. It consists of adding a medication with a different mechanism of action to the therapeutic regimen.
Lithium carbonate (Lithobid)
Lithium carbonate can be used as an effective augmenting agent in combination with an antidepressant in cases of treatment-resistant depression. It can also be used to treat or prevent episodes of depression. Lithium is contraindicated in patients with significant renal impairment.
It is important to note that lithium interacts with many drugs. Use of lithium often requires monitoring of lithium levels and renal and thyroid function tests.
Buspirone
Buspirone is marketed as an antianxiety medication; however, it may have antidepressant effects at doses above 45 mg/day. The antidepressant effects may increase when buspirone is used in combination with SSRIs and TCAs in patients with treatment-resistant depression. Buspirone is a partial 5-HT1A agonist with serotonergic and some dopaminergic effects in the CNS. It has anxiolytic effects but may take up to 2-3 weeks for full efficacy.
Serotonin-Dopamine Activity Modulators
Class Summary
Serotonin-dopamine activity modulators (SDAMs) act as a partial agonist at 5-HT1A and dopamine D2 receptors at similar potency, and as an antagonist at 5-HT2A and noradrenaline alpha1B/2C receptors. This mechanism of action is unique from other atypical antipsychotic drugs.
Brexpiprazole (Rexulti)
Serotonin-dopamine activity modulator (SDAM) indicated as an adjunct treatment for major depressive disorder. Dosage modifications are necessary with renal or hepatic impairment. Dosage modifications are also needed for individuals who are poor metabolizers of CYP2D6, or if coadministered drugs alter metabolism by CYP2D6 or CYP3A4.
Aripiprazole (Abilify, Abilify Discmelt)
Serotonin-dopamine activity modulator (SDAM) indicated as an adjunct treatment for major depressive disorder. Dosage modifications are also needed for individuals who are poor metabolizers of CYP2D6, or if coadministered drugs alter metabolism by CYP2D6 or CYP3A4. No dosage adjustment is required for renal or hepatic impairment.
Antidepressants, Other
Class Summary
Atypical antidepressants include bupropion (Wellbutrin, Wellbutrin SR), mirtazapine (Remeron), and trazodone (Desyrel). These agents are effective in treating major depression and may be effective in combination therapy in major depressive disorder. This group also shows low toxicity in overdose. Wellbutrin SR may have an advantage over the SSRIs by causing less sexual dysfunction and weight gain.
Bupropion (Wellbutrin, Aplenzin, Forfivo XL)
Bupropion inhibits neuronal dopamine reuptake and decreases the rate of norepinephrine activity. In addition to major depressive disorder, the indications for bupropion include smoking cessation. Off-label indications include attention-deficit/hyperactivity disorder and depression associated with bipolar disorder. Common side effects include headache and mild weight loss. Unlike other antidepressants, bupropion does not cause sexual dysfunction.
Mirtazapine (Remeron, Remeron SolTab)
Mirtazapine blocks both presynaptic and postsynaptic alpha-2 receptors but has a low affinity for alpha-1 receptors. It also blocks serotonin receptors 5HT2 and 5HT3. Common side effects include sedation, weight gain, and dry mouth.
Trazodone (Oleptro)
Trazodone is effective in the treatment of major depression. It inhibits the reuptake of serotonin and modulates serotonergic neurotransmission. It also significantly blocks histamine (H1) receptors. Its most common side effect is sedation, and thus, it has an off-label indication as a hypnotic. It can be very rarely associated with priapism, a medical emergency, and a dangerous side effect of this drug in men. It is often used at a low dosage (25 to 50 mg) as an adjunct to SSRIs to treat insomnia.
Stimulants
Class Summary
The CNS stimulants dextroamphetamine (Dexedrine) and methylphenidate (Ritalin) are sometimes used to augment antidepressants in patients with resistant depression.
Dextroamphetamine (Dexedrine, ProCentra, Zenzedi)
This is an augmenting agent in resistant depression. It has been studied most for treating patients who are medically ill and depressed. It is available as a sustained-release preparation.
Methylphenidate (Ritalin, Aptensio XR, Concerta, Daytrana, Metadate ER, Quillivant ER)
Methylphenidate has been mostly studied for treating patients who are medically ill and depressed. It is available as a sustained-release preparation.
Thyroid Products
Class Summary
Thyroid hormones liothyronine (T3, Cytomel) may modulate the effect of antidepressants.
Liothyronine (Cytomel, Triostat)
This synthetic salt of endogenous thyroid hormone may convert non-responders to antidepressants to responders by increasing receptor sensitivity and enhancing the effects of TCAs.
NMDA Antagonists
Class Summary
Studies have shown that the N-methyl-D-aspartate (NMDA) receptor may play a role in the pathophysiology of psychiatric disorders, including depression. The use of NMDA receptor antagonists has been shown to be effective in the treatment of the major depressive disorder.
Ketamine (Ketalar)
A non-competitive NMDA antagonist that blocks glutamate and has been found to have antidepressant effects. Ketamine is used off-label for treatment-resistant depression. By acting on the cortex and the limbic system, it produces a cataleptic-like effect state, which in turn causes the patient to feel dissociated from the surrounding environment.
Esketamine intranasal (Spravato)
Esketamine, the S-enantiomer of racemic ketamine, is a nonselective, noncompetitive N-methyl-D-aspartate (NMDA) receptor antagonist; the mechanism by which esketamine exerts its antidepressant effect is unknown.
In March 2019, the FDA approved Esketamine Nasal Spray for the treatment of treatment-resistant depression in conjunction with an oral antidepressant. It is also indicated for depressive symptoms in adults with major depressive disorder (MDD) with acute suicidal ideation or behavior with an oral antidepressant.
Esketamine is usually given under supervision with a newly initiated or optimized oral antidepressant, twice weekly for 4-weeks, at a dose of 84 mg.
Results from the trials showed that the active treatment significantly reduced depressive symptoms within 24 hours, with some patients starting to respond as early as 4-hours after the first dose.
Traditional oral antidepressants need weeks or more to take effect, so a drug that can begin providing relief within a day is potentially life changing.
“The clinical trials that support this new indication provide compelling evidence that Esketamine may offer clinicians a new way to support to patients quickly in an urgent depressive episode and help put them on the path to remission,” Gerard Sanacora, M.D., director of the Yale Depression Research Program, New Haven, Connecticut, and Esketamine clinical trial investigator, said in the same release.
A full course of treatment for MDD with acute suicidal ideation or behavior is twice weekly for 4-weeks, “after which evidence of therapeutic benefit should be evaluated to determine the need for continued treatment,” the company said.
Due to the risk for serious adverse events, including sedation and dissociation, and the potential for abuse or misuse, esketamine nasal spray is only available through a restricted distribution system — the Spravato Risk Evaluation and Mitigation Strategy (REMS).
The patient self-administers EsketamineNasal Spray only in REMS-certified healthcare settings. Patients are not permitted to take the drug home.
Natural treatments for depression

Traditional depression treatment uses a combination of prescription medication and counseling. But there are also alternative or complementary treatments you can try.
It is important to remember that many of these natural treatments have few studies showing their effects on depression, good or bad.
Likewise, the U.S. Food and Drug Administration (FDA) does not approve many of the dietary supplements on the market in the United States, so you want to make sure you are buying products from a trustworthy brand.
Talk to your healthcare provider before adding supplements to your treatment plan.
Supplements
Several types of supplements are thought to have some positive effects on depression.
Hypericum perforatum (St John’s Wort)
Although St. John’s Wort is considered a first-line antidepressant in many European countries, it has only recently gained popularity in the United States. Uses include treatment of mild to moderate depressive symptoms, but efficacy has not been demonstrated for major depression.
S-adenosyl-L-methionine (SAMe)
This compound has shown in limited studies to possibly ease symptoms of depression. The effects were best seen in people taking selective serotonin reuptake inhibitors (SSRIs), a type of traditional antidepressant.
5-hydroxytryptophan (5-HTP)
5-HTP may raise serotonin levels in the brain, which could ease symptoms. Your body makes this chemical when you consume tryptophan, a protein building block.
Omega-3 fatty acids
These essential fats are important to neurological development and brain health. Adding omega-3 supplements to your diet may help reduce depression symptoms.
Essential oils
Essential oils are a popular natural remedy for many conditions, but research into their effects on depression is limited.
People with depression may find symptom relief with the following essential oils:
- Wild Ginger: Inhaling this strong scent may activate serotonin receptors in your brain. This may slow the release of stress-inducing hormones.
- Bergamot: This citrusy essential oil has been shown to reduce anxiety in patients awaiting surgery. The same benefit may help individuals who experience anxiety because of depression, but there is no research to support that claim.
Other oils, such as chamomile or rose oil, may have a calming effect when they are inhaled. Those oils may be beneficial during short-term use.
Vitamins
Vitamins are important to many bodily functions. Research suggests two vitamins are especially useful for easing symptoms of depression:
- Vitamin B: B-12 and B-6 are vital to brain health. When your vitamin B levels are low, your risk for developing depression may be higher.
- Vitamin D: Sometimes called the sunshine vitamin because exposure to the sun supplies it to your body, Vitamin D is important for brain, heart, and bone health. People who are depressed are more likely to have low levels of this vitamin.
Many herbs, supplements, and vitamins claim to help ease symptoms of depression, but most have not shown themselves to be effective in clinical research.
Can Antidepressants Cause Erectile Dysfunction (ED)?
Sexual dysfunction is a side effect of many antidepressants. In men, this manifests as a reduction in sex drive (decreased libido) and difficulties developing and maintaining an erection.
Some antidepressants can also make it difficult to orgasm, while others, including citalopram, are linked to significant hormonal disruptions and a large reduction in sperm count.
Sexual side effects such as ED are a side effect of almost all antidepressants, including all the drugs listed below:
- Citalopram
- Sertraline
- Fluoxetine
- Paroxetine
- Duloxetine
- Escitalopram
If you are prescribed one of these medications and have noticeable sexual side effects such as erectile dysfunction, it could potentially be a side effect of the antidepressant.
How Antidepressants Can Cause ED
Most antidepressants are selective serotonin reuptake inhibitors (SSRIs), a class of drugs that treat depression and anxiety disorders by increasing the amount of serotonin in the body. Some SSRIs have been shown to cause sexual issues for up to 60 percent of patients that take them on a regular basis.
Serotonin is a neurotransmitter that contributes to feelings of happiness and wellbeing, making it important in the treatment of depression, anxiety, panic disorders, eating disorders, and a variety of other conditions.
In addition to producing feelings of calmness and relaxation, serotonin and erectile dysfunction are linked because it can also result in lower levels of sexual interest.
According to one recent study, SSRI users notice an impact on the feelings of love and attachment they experience towards their romantic partner.
SSRIs also have a direct effect on many of the hormones that regulate sexual behavior in both men and women.
For example, many SSRIs cause an increase in prolactin — a hormone that can make it more difficult for men to orgasm and is linked to post-coital sleepiness. Animal studies also suggest that SSRIs can reduce testosterone levels, resulting in a weaker libido.
In short, there are numerous ways in which SSRIs and other antidepressants can affect your sex life. From reduced libido to difficulty orgasming, this class of drug is linked to a range of sexual side effects that can differ from person to person.
Do You Have ED from Using Antidepressants?
The association between antidepressants and erectile dysfunction is clear. If you take antidepressants and have erectile dysfunction, it is important to talk to your healthcare provider before you consider using medication to treat your ED.
Not all antidepressants have the same side effect profile, meaning your healthcare provider may be able to recommend an alternative medication that treats your depression or anxiety symptoms without the same impact on your sexual desire and performance.
Alternatively, your healthcare provider might recommend adjusting your antidepressant dosage, which can—in some cases—reduce or eliminate the sexual side effects caused by the medication.
Finally, there is the option of using ED drugs like sildenafil, tadalafil, or vardenafil. As always, it is best to discuss this with your healthcare provider to learn more about how these drugs can be used safely in conjunction with your depression or anxiety medication. You may find it is not as simple as asking, “Can you take Viagra with antidepressants?”
Can ED Drugs Solve SSRI-Induced Sexual Dysfunction?
Erectile dysfunction medications such as sildenafil have proven useful in treating many of the sexual side effects caused by SSRIs.
One study from 1999 involved 14 male patients, all of whom experienced sexual dysfunction from SSRI use. The patients were given 25mg to 100mg tablets of sildenafil, which they took just before sexual activity.
Thirteen out of the 14 patients, all of whom previously reported sexual dysfunction, experienced an improvement after using sildenafil. Most saw a noticeable improvement at the smallest 25mg dose, while others required a 75mg or 100mg dosage for noticeable results.
In short, drugs like sildenafil appear to work very well in treating erectile dysfunction caused by antidepressants.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment.




