Stroke Risk Factors Unique to Women
Stroke is the third leading cause of death in women in the United States and is a leading cause of disability. Each year 55 000 more women than men have a stroke, a discrepancy largely driven by longer life expectancy in women. Although the majority of stroke incidence can be attributed to traditional vascular risk factors that occur in both men and women, including hypertension, hyperlipidemia, diabetes mellitus, smoking, and atrial fibrillation, there are several stroke risk factors that are specific to women. Specifically, differences in sex hormones, exogenous estrogens, and pregnancy exposures are factors exclusively experienced by women. In this review, we will summarize women-specific factors, such as endogenous hormone levels, exogenous hormone therapy, pregnancy, parity, the timing of age at menarche, and menopause in relation to stroke risk.
Endogenous Estrogen State
Estrogen levels fluctuate dramatically in women with the menstrual cycle and then drop dramatically in the menopausal transition and in post-menopause. In data from the Copenhagen City Study, neither high nor low estradiol levels were associated with increased risk of ischemic stroke. In the Study of Osteoporotic Fractures, women in the highest category of free estrogen index had a higher age-adjusted risk of ischemic stroke, but this was not independent of standard stroke risk factors, including hypertension, diabetes mellitus, and adiposity. Subsequently, a meta-analysis of the available studies found no association, further supporting the lack of a relationship between estradiol levels and risk of ischemic stroke.
Testosterone
Testosterone levels are more stable than estrogen levels across the lifespan in women, with relatively constant levels from ages 30 to 70 years. Although low testosterone levels have been associated with increased stroke risk in men, no clear relationship has been seen for testosterone levels and risk of stroke in women. A study of French women over the age of 65 years found no association between high or low testosterone levels and risk of stroke.
Dehydroepiandrosterone, an adrenal hormone which can also be used for the synthesis of estrogen and testosterone, has also been investigated. Low dehydroepiandrosterone levels have been associated with increased risk of ischemic stroke, with women in the lowest quartile having a relative risk (RR) of 1.41 (95% confidence interval [CI], 1.03–1.92) for ischemic stroke after adjustment for other risk factors. Dehydroepiandrosterone levels at the presentation of acute stroke were also inversely associated with stroke severity in a hospital-based study of stroke in postmenopausal women. Another study of women undergoing coronary angiography provided evidence that lower dehydroepiandrosterone levels were associated with increased cardiovascular mortality, including death from stroke.
Age at Menarche
Earlier age at menarche has been associated with greater cardiovascular disease (CVD) morbidity and mortality. In the Million Women Study from the United Kingdom, a U-shaped relationship between age at menarche and cerebrovascular disease was observed. Women who experienced menarche at age ≤ 10 years were at higher risk of developing stroke in later life compared with those with age at menarche at 13 years; however, women who experienced menarche at age ≤ 7 years were also at higher risk of developing stroke compared with those with age at menarche at 13 years. Women with extremely early age at menarche may experience hormonal disturbances, such as higher exposure to estradiol, potentially mediated through childhood obesity. The timing of menarche is associated with type 2 diabetes mellitus risk, an association which may be influenced by childhood adiposity and endocrinopathies. Although the Million Women Study attempted to control for potential confounding factors, such as body mass index, through statistical adjustment, obesity may have been present before the onset of menarche, complicating inferences about cause and effect.
Age at Natural Menopause and Surgical Menopause
Women of reproductive age are at a lower risk of CVD compared with men of similar age and lifestyle, but women who experience early menopause have increased cardiovascular risk. Early age at natural menopause (menopause onset before 45 years) was associated with a slightly higher risk of total CVD mortality than onset at age 45 years or later; however, this association was not observed for stroke mortality risk independently. Surgical menopause, bilateral oophorectomy with or without hysterectomy, has also been associated with a higher risk of CVD. In the Nurses’ Health Study, bilateral oophorectomy before age 50 years was associated with increased CVD mortality in women and especially in women who did not use hormone therapy.
Specific mechanisms responsible for the association between the timing of age at menopause and CVD are unclear. However, CVD incidence rising sharply after menopause suggests the protective benefits of ovarian hormones. Estrogen inhibits hepatic lipase, thus decline in endogenous estrogens in the menopausal transition may adversely affect lipid levels and subsequently cardiovascular risk. The menopausal transition is associated with declines in high-density lipoprotein cholesterol and increases in low-density lipoprotein cholesterol, as well as changes in high-density lipoprotein composition, with a higher number of small high-density lipoprotein particles, which confer less cardiovascular protection than large high-density lipoprotein particles. Hence, decreased estrogen concentrations over the menopause transition and effects on lipoprotein profiles may subsequently contribute to atherosclerosis. In the prospective cohort Nurses’ Health Study, a shorter duration of reproductive lifespan was associated with a higher risk of stroke, as well as CVD, which was likely driven by an earlier age at menopause (either naturally or surgically).
Exogenous Estrogens and Stroke Risk
Hormone-containing Birth Control and Stroke
Hormonal contraceptives, including oral, transdermal, and vaginal formulations, are effective and are used worldwide by more than 100 million women. There are various formulations containing either combined estrogen and progestogen or progestogen alone, administered as pills, patches, and rings. Combined oral contraceptives (COC), comprised both estrogen and progestogen, are thrombogenic and, historically, have been associated with increased risk of CVD. Oral estrogens have a dose-response association with risk, and doses have declined since their introduction in the 1960s. Most COCs now contain <50 μg and some contain as low as 15 μg of estrogen. Authors who evaluated the risk of second- and third-generation estrogen-containing oral contraceptives continued to find a 60% to 80% increased odds of the combined endpoint of myocardial infarction or ischemic stroke among COC users compared with nonusers. Progestogen-only hormonal contraceptives have not been associated with increased risk of ischemic stroke although data are limited. Nonoral methods of delivering combined hormonal contraceptives, including the vaginal ring and contraceptive patches, seem to have the same risk as oral contraceptives.
Risk of stroke with COC use rises in the presence of other cardiovascular risk factors (i.e., smoking, age >35 years, and a history of migraine with aura). Migraine with aura is a common condition in younger women, and the risk of stroke in patients with migraine with aura is increased 2-fold. Women with migraine who also use COCs have a further increased risk of ischemic stroke, where women with migraine with aura, COC use, and who are active smokers have a dramatically elevated risk for stroke. Women who have migraine with aura should be advised to control all modifiable risk factors, including tobacco use, hypertension, and birth control methods other than COCs should be considered.
Hormonal contraceptives are used by millions of women, and for most low-risk women, the risk of stroke associated with COC is lower than the risk of stroke during pregnancy. However, there is a clear association between hormone-containing birth control methods and ischemic stroke. This is magnified by stroke risk factors. Although a COC pill containing 30 μg of estrogen is considered safe and effective hormonal contraception, careful attention to stroke risk should be made before prescribing. Nonhormonal and progestogen-only methods of contraception should also be considered in high-risk patients.
Postmenopausal Hormone Therapy and Stroke Risk
Prospective observational studies and randomized trials consistently demonstrate an increased risk of stroke, particularly ischemic stroke, with oral postmenopausal hormone therapy.
In prospective cohort studies, data suggest that postmenopausal users of oral estrogens with or without progestin have a 27% to 39% increased risk of stroke compared with nonusers.
Although some data suggest an association between timing of hormone therapy and coronary heart disease, time since menopause is not associated with differences in stroke incidence in either observational studies or clinical trials. The incidence of stroke is relatively low in younger women (age, 50–59 years), with 2- additional cases of stroke per 10 000 women per year taking postmenopausal hormones. In addition, there is a dose-response relationship between the dose of oral conjugated estrogen and stroke, with RRs of 0.93 for a dose of 0.3 mg, 1.54 at 0.625 mg, and 1.62 at 1.25 mg (P for trend, <0.001).
Limited data are available for transdermal estrogens, which have been associated with a lower risk of venous thromboembolism. In a population-based case control study, current use of transdermal hormone therapy was not associated with an increased risk of stroke. However, when the dose was examined, low-dose transdermal estrogen (less than or equal to 50 μg/d estradiol) was not associated with risk while high-dose transdermal estrogen (>50 μg/d) was associated with increased stroke risk.
Transgender Medicine
Transgender individuals are people whose sex identity differs from their sex assigned at birth. The prevalence of self-identified transgender adults in the United States is estimated to be 0.5% of the population. Some transgender people pursue hormonal therapy or sex-affirming surgery to assume secondary sex characteristics consistent with their sexual identity. The use of certain hormonal therapies has implications for the incidence of cerebrovascular disease in these individuals.
Transwomen are people with assigned male sex and female sex identity. Transwomen may undergo medical treatment with estrogens, antiandrogens, or a combination of both. Those who have undergone orchiectomy may pursue only estrogen therapy.
Antiandrogen therapies do not seem to increase stroke risk in transwomen. Spironolactone is the antiandrogen most commonly prescribed to transwomen in the United States. Spironolactone, a potassium-sparing diuretic, may lower blood pressure but does not increase thrombotic risk. Similarly, finasteride, a less commonly used antiandrogen, does not seem to increase thrombotic risk.
Direct data on the effect of exogenous estrogens in transwomen are scant. Much of our knowledge about the effects of exogenous estrogen is derived from studies of the increased risk of thrombotic complications, including stroke among postmenopausal women using postmenopausal hormone therapy. Prospective trials of thrombotic risk in transwomen receiving estrogen therapy are lacking. A 1997 Dutch single-center retrospective descriptive study of 816 transwomen treated for a mean 9.5 patient-years with ethinyl estradiol and the antiandrogen cyproterone acetate found that 45 (5.5%) developed deep vein thrombosis or pulmonary embolism, 5 (0.6%) experienced a transient ischemic attack, and none experienced an ischemic stroke. A 2013 Belgian single-center case-control study evaluated 214 transwomen who were maintained on estrogen therapy for a median of 6 years. Eleven of the 214 transwomen (5.1%) developed deep vein thrombosis or pulmonary embolism during hormonal treatment. Five of the 214 transwomen (2.3%) were diagnosed with a transient ischemic attack or cerebrovascular disease during treatment, a higher prevalence than in the age-matched control men. In a 2011 Dutch retrospective single-clinic cohort mortality study of 966 transwomen on estrogen with or without antiandrogen therapy with a mean follow-up of 19.4 years, no difference was found in the incidence of fatal stroke in transwomen compared with the incidence in the general population.
As we await prospective studies of estrogen therapy in transwomen, medical providers should maintain a high index of suspicion for deep vein thrombosis/pulmonary embolism and cerebral venous thrombosis in transwomen receiving estrogen therapy. Cardiovascular risk should be evaluated, and transwomen who smoke should be encouraged to quit smoking and provided with appropriate pharmacological and psychosocial supports.
Transmen are individuals with assigned female sex and male sexual identity. Transmen may undergo treatment with testosterone to promote the development of male secondary sex characteristics. Testosterone is available via transdermal and intramuscular routes. Unlike estrogen, testosterone does not seem to be associated with an increased risk of thromboembolic complications. The majority of existing studies of transmen do not suggest an increased risk of cardiovascular morbidity with exogenous testosterone therapy.
In general, providers should be aware that transgender people may be less likely to seek medical attention than their cisgender peers because of previous negative interactions with the medical community, poor psychosocial wellbeing, and fear of stigma. This has direct implications for the delay of appropriate stroke care. Health systems and medical providers can improve the medical care of transgender people by asking about sexual identity and preferred pronouns on intake forms; promoting an explicitly supportive and inclusive clinic or unit culture for transgender patients and their families and pursuing research into the unique health needs of transmen and transwomen.
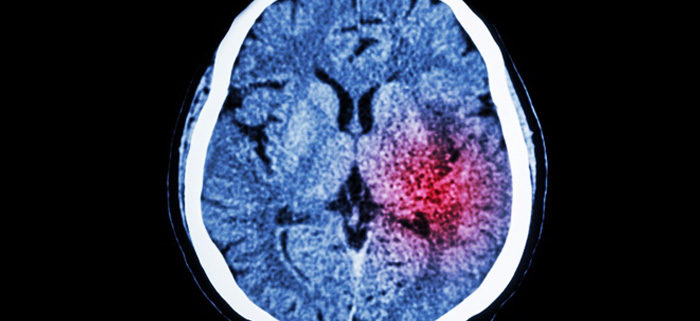
Issues of Pregnancy, Parity, and Stroke
Pregnancy and the peripartum are associated with increased risk of stroke. The peripartum period from 2 days before to 1 day after delivery and, to a lesser extent, up to 6 weeks postpartum is associated with an increased risk of ischemic stroke and intracerebral hemorrhage. In a large population-based study of women in England (age, 15–49 years), the baseline incidence of stroke was 25.0/100 000 person-years in women when they were not pregnant. The incidence rate dropped during early pregnancy but was 9-fold higher in the peripartum period (161.1/100 000 person-years) and 3-fold higher in the early postpartum period (47.1/100 000 person-years). For subarachnoid hemorrhage, only the peripartum period confers increased risk; nonaneurysmal subarachnoid hemorrhage is likely a major contributor to this risk. The risk of any thrombotic event that includes ischemic stroke remains increased to a lesser extent until 12- weeks postpartum, but it is not established that the risk of stroke remains increased beyond 6-weeks postpartum. Eclampsia and preeclampsia are the strongest risk factors for both ischemic stroke and intracerebral hemorrhage accounting for 24% to 48% of all pregnancy-associated strokes; this risk is potentiated by preexisting genitourinary tract infection, chronic hypertension, prothrombotic states, and coagulopathies.
Complications of pregnancy, specifically pregnancy-induced hypertension, gestational diabetes mellitus, and preeclampsia, are also associated with long-term risk of stroke. There is evidence that women with pregnancy outcomes of preterm birth and small for gestational age infants have higher rates of cerebrovascular events even after adjusting for other pregnancy complications.
For women with prior stroke, the risk of recurrent stroke is increased in the peripartum and postpartum periods. Limited data from case series suggest an absolute risk of recurrent arterial ischemic stroke associated with the pregnancy of 0.7%, similar to the <1% yearly risk of recurrent stroke among young adults who have no vascular risk factors. In addition, the absolute risk depends on clinical circumstances, with the presence of vascular risk factors or a definite cause of stroke, including thrombophilic disorders, conferring increased risk. Similarly, there is a paucity of information on the excess risk of pregnancy complications to mother and child among women with prior ischemic stroke.
Conclusions
It is important to be aware of stroke risk factors specific to women. Specific considerations that include endogenous hormone levels, exogenous hormone therapy, pregnancy and the peripartum period, and pregnancy-related complications, change the risk of stroke for women as well as the optimal stroke prevention strategies. Special attention and further research are also needed in the area of transgender individuals.


Leave a Reply
Want to join the discussion?Feel free to contribute!