Stroke
Stroke (also known as cerebrovascular accident [CVA]) is an acute interruption of blood flow to a portion of the brain, resulting in cell death and loss of associated neurologic function in the affected areas.
Stroke is the fifth leading cause of death in the United States. Someone in the United States dies from a stroke every four minutes, according to the American Stroke Association. Stroke is also the leading cause of disability. Stroke victims who survive may suffer a variety of neurological deficits that can lead to paralysis, loss of speech and vision, memory problems, cognitive deficits, emotional problems, and more.
Transient Ischemic Attack (TIA)
A transient ischemic attack (TIA) is an acute episode of temporary neurologic dysfunction that results from focal cerebral, spinal cord, or retinal ischemia, and is not associated with acute tissue infarction.
TIAs are often labeled “mini-strokes,” because they can be relatively benign in terms of immediate consequences. The term “warning stroke” is more appropriate for these temporary episodes, because a TIA can signal a problem that may lead to further strokes, disability, or even death.
Even though TIA symptoms usually last less than five minutes with an average of about a minute, with no noticeable or lasting effects, anyone who has symptoms should be rushed to the emergency room.
When stroke symptoms are first noticed, it isn’t safe to assume they will disappear without urgent medical care. Trained medical staff should evaluate the patient’s condition. Some signs are only visible with hospital equipment, so appropriate medical care is important.
Types of Stroke
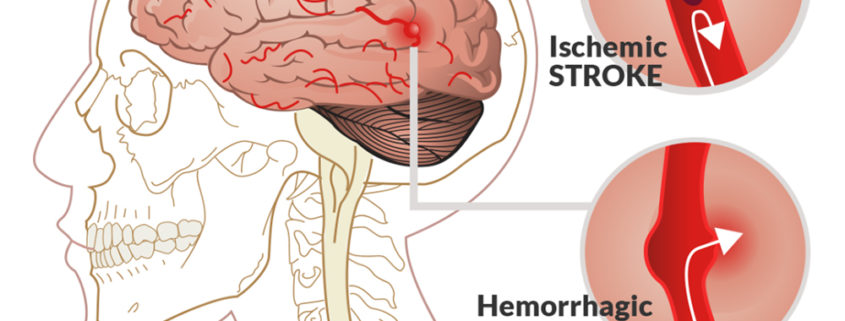
There are two basic types of stroke: ischemic (caused by a blood clot) and hemorrhagic (caused by bleeding). It is critical for a doctor not only to quickly determine whether a patient is suffering from a stroke, but also to quickly determine the type of stroke. The medication for one type can negatively affect a patient suffering from the other type.
Ischemic Stroke
Nearly 800,000 people suffer strokes each year in the United States; 87% of these strokes are ischemic.
Ischemic strokes occur as a result of an obstruction within a blood vessel supplying blood to the brain. The underlying condition for this type of obstruction is the development of fatty deposits lining the vessel walls. This condition is called atherosclerosis. These fatty deposits can cause two types of obstruction:
- Cerebral thrombosis refers to a thrombus (blood clot) that develops at the clogged part of the vessel.
- Cerebral embolism refers generally to a blood clot that forms at another location in the circulatory system, usually the heart and large arteries of the upper chest and neck. A portion of the blood clot breaks loose, enters the bloodstream and travels through the brain’s blood vessels until it reaches vessels too small to let it pass. A second important cause of embolism is an irregular heartbeat, known as atrial fibrillation. It creates conditions where clots can form in the heart, dislodge and travel to the brain.
Ischemic strokes occur as a consequence of thromboembolic occlusion of cerebral arteries. Occlusion of blood flow begins an ischemic cascade that, if unchecked, will result in irreversible infarction; hypoxia-induced cell death causes inflammatory swelling, which may alter the brain architecture, producing a midline shift.
Hemorrhagic Stroke
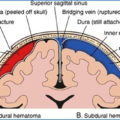
Hemorrhagic stroke results from a weakened vessel that ruptures and bleeds into the surrounding brain. The blood accumulates and compresses the surrounding brain tissue. The two types of hemorrhagic strokes are intracerebral (within the brain) hemorrhage or subarachnoid hemorrhage.
Two types of weakened blood vessels usually cause hemorrhagic stroke: aneurysms and arteriovenous malformations (AVMs).
- An aneurysm is a ballooning of a weakened region of a blood vessel. If left untreated, the aneurysm continues to weaken until it ruptures and bleeds into the brain.
- An arteriovenous malformation (AVM) is a cluster of abnormally formed blood vessels. Any one of these vessels can rupture, also causing bleeding into the brain.
Although intracerebral hemorrhage is less common than ischemic stroke, it is often more serious, with many patients dying within a month of an intracerebral hemorrhage. A subarachnoid hemorrhage results from the bleeding of an artery around the base of the brain. It is the least common type of stroke, accounting for about 5 percent of all strokes.
Patients with hemorrhagic strokes present similarly to those with ischemic strokes, except that they tend to appear more ill, with signs of increased intracranial pressure. Ischemic and hemorrhagic strokes cannot be reliably differentiated on the basis of clinical examination findings alone. Further evaluation, especially with brain imaging tests, are necessary.
Silent Cerebral infarction
Silent cerebral infarction (SCI), or “silent stroke,” is a brain injury likely caused by a blood clot interrupting blood flow in the brain. It’s a risk factor for future strokes which could lead to progressive brain damage due to these strokes.
Brain Stem Stroke
Brain stem strokes can have complex symptoms, and they can be difficult to diagnose. A person may have vertigo, dizziness and severe imbalance without the hallmark of most strokes – weakness on one side of the body. The symptoms of vertigo, dizziness or imbalance usually occur together; dizziness alone is not a sign of stroke. Brain stem stroke can also cause double vision, slurred speech and decreased level of consciousness.
Only a half-inch in diameter, the brain stem controls all basic activities of the central nervous system: consciousness, blood pressure, and breathing. All of the motor control for the body flows through it. Brain stem strokes can impair any or all of these functions. These complications are often predictable and, with prompt recognition, can be treated. If complications are dealt with quickly, there is a good chance of recovery.
More severe brain stem strokes can cause locked-in syndrome, a condition in which survivors can move only their eyes.
If a stroke in the brain stem results from a clot, the faster blood flow can be restored in this critical area, the better the chances for recovery. It is important that the public and healthcare professionals know all of the symptoms of a stroke and are aware that some brain stem strokes have distinct symptom.
Like all strokes, brain stem strokes produce a wide spectrum of deficits and recovery. Whether a survivor has minor or severe deficits depends on the location of the stroke within the brain stem, the extent of injury and how quickly treatment is provided.
Risk factors for brain stem stroke are the same as for strokes in other areas of the brain: high blood pressure, diabetes, heart disease, atrial fibrillation and smoking. Like strokes in other areas of the brain, brain stem strokes can be caused by a clot or a hemorrhage. There are also rare causes, like injury to an artery due to sudden head or neck movements.
Dramatic recovery from a brain stem stroke is possible. Because brain stem strokes do not usually affect language ability, the patient is able to participate more fully in rehabilitation therapy. Most deficits are motor-related, not cognitive. Double vision and vertigo commonly resolve after several weeks of recovery in mild to moderate brain stem strokes.
Stroke in Children
Stroke in children is rare but should be considered as a possible diagnosis in any child with a headache and new-onset focal neurologic symptoms or signs. Children are much more likely than adults to have a headache at onset of ischemic stroke.
Stroke diagnosis in children is confounded by stroke “mimics,” most commonly migraine with aura, followed by Bell’s palsy and conversion disorder. Urgent brain imaging may be required to distinguish a migraine with aura from a stroke.
Among 355 children (age 29 days to 18 years) with ischemic stroke enrolled in the multicenter Vascular Effects of Infection in Pediatric Stroke (VIPS) study, headache was uncommon in children younger than 3 years (5 of 90 [6%]) but was present in nearly half of those aged 3 years and older (108 of 265 [46%]). It should be noted that children younger than 3 years may not be able to communicate about whether they are having a headache.
In children aged 3 years and older, infarcts occurred most often in the posterior cerebral artery (23%) and superior cerebellar artery (13%). Nearly half of infarcts occurred on the right side (48%).
Risk Factors for Stroke
Stroke risk factors that can be modified and improved:
High blood pressure
Hypertension is the leading cause of stroke and the most significant controllable risk factor for stroke.
Smoking
Recent studies confirm that cigarette smoking is another crucial risk factor for stroke. The nicotine and carbon monoxide in cigarette smoke damage the cardiovascular system and pave the way for a stroke to occur. Additionally, the use of birth control pills combined with cigarette smoking can greatly increase the risk of stroke.
Diabetes
Diabetes Mellitus is an independent risk factor for stroke. Many people with diabetes also have high blood pressure, high blood cholesterol and are overweight. This increases their risk even more. While diabetes is treatable, the presence of the disease still increases risk of stroke.
Diet
Diets high in saturated fat, trans fat and cholesterol can raise blood cholesterol levels. Diets high in sodium (salt) can increase blood pressure. Diets with high calories can lead to obesity. Also, a diet containing five or more servings of fruits and vegetables per day may reduce the risk of stroke.
Physical Activity
Physical inactivity can increase the risk of stroke, heart disease, becoming overweight, developing high blood pressure, high blood cholesterol, diabetes, heart disease and stroke.
Obesity
Excess body weight and obesity are linked with an increased risk of high blood pressure, diabetes, heart disease and stroke.
High Blood Cholesterol
People with high blood cholesterol have an increased risk for stroke. Large amounts of cholesterol in the blood can build up and cause blood clots, leading to a stroke. Also, it appears that low HDL (“good”) cholesterol is a risk factor for stroke in men, but more data is needed to verify if this is true for women as well.
Carotid Artery Disease
The carotid arteries supply blood to the brain. A carotid artery narrowed by plaque may predispose to thrombus formation. Because they’re located so close to the brain, carotid arteries may more easily cause a stroke, but any artery disease may contribute to a stroke.
Peripheral Artery Disease
PAD is the narrowing of blood vessels carrying blood to leg and arm muscles. It’s caused by fatty buildups of plaque in artery walls. People with peripheral artery disease have a higher risk of carotid artery disease, which raises their risk of stroke.
Atrial Fibrillation
AFib (a heart rhythm disorder) increases stroke risks fivefold. That’s because it causes the heart’s upper chambers to beat incorrectly, which can allow the blood to pool and a clot to travel to the brain and cause a stroke. Also, sleep apnea can be linked to AFib and is associated with increased stroke risks.
Other Heart Disease
People who have coronary heart disease or heart failure are at higher risk of stroke than people who have healthy hearts. Dilated cardiomyopathy (an enlarged heart), heart valve disease and some types of congenital heart defects can also raise the risk of stroke.
Sickle Cell Disease
This treatable genetic disorder mainly affects African-American and Hispanic children. “Sickled” red blood cells are less able to carry oxygen to the body’s tissues and organs. These cells also tend to stick to blood vessel walls, which can block arteries to the brain and cause a stroke.
Stroke Risk Factors that Are Not Subject to Control
You can’t control some risk factors, but knowing that they exist may help motivate you to work harder on the ones you can change.
- Age matters. The likelihood of having a stroke nearly doubles every 10 years after age 55. Although stroke is more common among the elderly, a lot of people under 65 also have strokes. Even babies and children can sometimes have a stroke.
- A family history of stroke can raise your risk. If your parent, grandparent, sister or brother has had a stroke — especially before reaching age 65 — you may be at greater risk. Sometimes strokes are caused by genetic disorders like CADASIL, which can block blood flow in the brain.
- Race can make a difference. Statistics show that African-Americans have a much higher risk of death from a stroke than Caucasians do. This is partly because blacks have higher risks of high blood pressure, diabetes and obesity. Hispanics and Latinos also have unique risks for stroke.
- Sex (gender) can affect stroke risks. Each year, women have more strokes than men, and stroke kills more women than men, too. Factors that may increase stroke risks for women include: pregnancy, history of preeclampsia/eclampsia or gestational diabetes, oral contraceptive use (especially when combined with smoking) and post-menopausal hormone therapy.
- Prior stroke, TIA or heart attack can raise risk. A person who has had a prior stroke has a much higher risk of having another stroke than a person who has never had one. TIAs are also strong predictors of stroke. A person who’s had one or more TIAs is almost 10 times more likely to have a stroke than someone of the same age and sex who hasn’t. TIAs should be considered a medical emergency and followed up immediately with a healthcare professional.
Additional Factors that May Be Linked to Higher Stroke Risks
- Geographic location can make a difference. Strokes are more common in the southeastern United States than in other areas. These are the so-called “stroke belt” states. Check out your state and consider how it supports healthy habits.
- Socioeconomic factors may have an impact. There’s some evidence that strokes are more common among those with lower incomes. One reason may be because smoking and obesity rates are also higher. Another reason may be that access to quality healthcare is often more limited at lower income levels.
- Alcohol abuse can raise stroke risk. In fact, in can lead to medical complications, including stroke. If you drink alcohol, we recommend no more than two drinks per day for men and no more than one drink per day for non-pregnant women, based on current evidence for lowering stroke risk. .
- Drug abuse is associated with increased risk. The most commonly abused drugs, including cocaine, amphetamines and heroin, have been associated with an increased risk of stroke. Drug addiction is often a chronic relapsing disorder associated with a number of societal and health-related problems. Strokes caused by drug abuse are often seen in a younger population.
- Sleep habits can affect stroke risk factors. Recent studies have begun to clarify the reasons that people who get regular, good quality sleep tend to have lower heart disease and stroke risks.
Whether your risks are related to changeable factors or are primarily outside of your control, you can benefit your heart and your brain with healthy lifestyle choices.
Symptoms & Signs of Stroke
FACE DROOPING
Does one side of the face droop or is it numb? Ask the person to smile. Is the person’s smile uneven or lopsided?
ARM WEAKNESS
Is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward?
SPEECH DIFFICULTY
Is speech slurred? Is the person unable to speak or hard to understand? Ask the person to repeat a simple sentence, like “The sky is blue.” Is the person able to correctly repeat the words?
TIME TO CALL 9-1-1
If someone shows any of these symptoms, even if the symptoms go away, call 9-1-1 and say, “I think this is a stroke” to help get the person to the hospital immediately. Time is important! Don’t delay, and also note the time when the first symptoms appeared. Emergency responders will want to know.
Beyond F.A.S.T. – Other Symptoms include:
- Sudden NUMBNESS or weakness of face, arm, or leg, especially on one side of the body
- Sudden CONFUSION, trouble speaking or understanding speech
- Sudden TROUBLE SEEING in one or both eyes
- Sudden TROUBLE WALKING, dizziness, loss of balance or coordination
- Sudden SEVERE HEADACHE with no known cause
Proper Diagnostic Procedure for Stroke
In most cases, an emergency room or urgent care provider is the first medical professional to evaluate a patient who is experiencing a stroke. They must act quickly to be effective, as brain cells begin to die within minutes of being deprived of oxygen. Prompt recognition and treatment of stroke can restore blood flow to affected areas and minimize brain damage and potential complications.
To diagnose a stroke, a provider should obtain a good medical history, including medications the patient is taking, and risk factors for stroke, such as high blood pressure, heart disease, high cholesterol, diabetes, smoking, and an unhealthy lifestyle.
A patient suffering a stroke may not be able to perceive the symptoms or communicate them to a provider, as this condition affects the brain. This makes it critically important for the provider to recognize the symptoms of stroke and correctly diagnose it.
Common signs and symptoms of stroke vary depending upon the regions of the brain that are compromised. An anterior circulation stroke involves a branch of the internal carotid artery and can result in aphasia, unilateral motor and sensory deficits, or hemineglect. Vertebrobasilar infarct symptoms include decreased level of consciousness, cranial nerve deficits, and motor and sensory deficits, including quadriparesis, nystagmus, visual changes and visual field deficits, ataxia, and vertigo.
The provider should also conduct neurologic tests (right-and left-side strength and ability to comply) and ask about the onset of symptoms, since stroke occurs rapidly and mimicking conditions often do not.
Several tests are available to assist with diagnosis, including blood tests (which can rule out infections as well as blood-sugar and other chemical imbalances). For example, if the doctor believes that the stroke was caused by a blood clot, the doctor may order a series of blood tests to determine how to prevent future clots.
The primary means of distinguishing stroke from other ailments is brain imaging, including CT Scan and MRI. Those tests should reveal whether a patient is suffering from a stroke and what type of stroke it is, or show evidence of tumors or other problems. But because the images are not always conclusive, doctors can make mistakes even after the proper tests have been performed. A misdiagnosis can come in the form of either failing to properly determine the type of stroke, or as diagnosing a stroke as some other illness.
Imaging Studies
Non-contrast CT scanning of the head is the first-line imaging modality in the assessment of a suspected stroke. It is employed primarily to exclude intracranial hemorrhage or a stroke mimic, which would preclude the administration of thrombolytic therapy. CT scanning is insensitive for ischemic stroke within the first 6-12 hours because edema and infarction have not yet developed enough to be identified; therefore, a normal CT scan does not rule out the possibility of an ischemic stroke. However, CT scanning is highly sensitive for detecting intracranial hemorrhage, which appears as a readily identifiable, hyperdense area within the brain.
MRI
MRI is more sensitive for the detection of early brain injury than CT scanning, although CT scanning remains the test of choice in most acute stroke patients within the window for treatment, due to its comparative speed, availability, and lack of contraindications.
Diffusion-weighted imaging (DWI), a form of MRI, detects the free motion of water particles, which becomes restricted in the presence of cell death and cytotoxic edema. DWI can detect injury within 15-30 minutes of symptom onset. An evidence-based guideline from the American Academy of Neurology advises that DWI is more useful than non-contrast CT scanning for the diagnosis of acute ischemic stroke within 12 hours of symptom onset and should be performed for the most accurate diagnosis of acute ischemic stroke. DWI is also ideal for detecting very small areas of ischemia that are imperceptible on CT scans.
Both CT scanning and MRI are sensitive for intracerebral blood products. MRI has the added advantage of being useful for estimating the age of the hemorrhage if this cannot be determined clinically. Hyperacute blood appears isointense to the brain on T1- and T2-weighted imaging, whereas acute blood (1-2 days) appears dark on T-2 weighted imaging and isointense on T1-weighted imaging. As blood continues to age, the signal characteristics change. Early subacute blood (2-7 days) appears bright on T1-weighted imaging and dark on T-2 weighted imaging; late subacute blood (7-28 days) appears bright on T1- and T2-weighted imaging, and chronic hemosiderin appears dark on T1- and T2-weighted imaging.
Perfusion-weighted imaging (PWI) enables detection of at-risk brain tissue by directly measuring tissue perfusion. The routine use of perfusion imaging in acute stroke is controversial at this time.
Angiography
Evaluation of the cerebral vasculature can be performed by means of CT angiography (CTA), MR angiography (MRA), or conventional angiography. Conventional angiography offers the highest spatial resolution, but it carries a fixed (albeit low) risk of stroke. Both CTA and MRA perform well at identifying large vessel occlusions, and CTA has the added benefits of speed and good spatial resolution. Use of the postprocessing 3D workstations allows radiologists to create rendered images that can readily demonstrate areas of occlusions or aneurysmal dilation.
As part of the evaluation of a stroke patient, MRA is typically performed in conjunction with standard brain MRI. Because of its lower spatial resolution, MRA is not as sensitive as CTA, or conventional angiography, but it can be helpful in correlating associated MRI findings from DWI.
Conventional angiography is typically performed if an endovascular intervention is to be carried out. Such intervention would include endovascular therapy for treatment of acute ischemic stroke or evaluation and treatment of an aneurysm identified on CTA or MRA. Of all the imaging modalities employed in this setting, conventional angiography offers the best spatial resolution; it also allows therapeutic intervention. Unfortunately, as mentioned, there is a small risk of stroke secondary to the intervention.
Misdiagnosis of Stroke
A doctor may misdiagnose a patient with stroke-like symptoms even after imaging tests have been conducted. A misdiagnosis can come in the form of either failing to properly determine the type of stroke, or as diagnosing a stroke as some other illness. Below are a few illnesses that may be challenging to differentiate from a stroke:
Bell Palsy
It is no surprise that Bell palsy is sometimes confused with stroke. Public awareness campaigns, such as the National Stroke Association’s Act FAST (face, arms, speech, time), highlight facial droop and dysarthria as reasons to rush a patient to the hospital for treatment with tissue plasminogen activator (tPA).
Bell palsy is characterized by unilateral facial droop that, if severe enough, may cause difficulty speaking. However, facial weakness from Bell palsy is due to lower motor neuron dysfunction, whereas facial weakness from a stroke usually stems from upper motor neuron impairment. (In rare cases, a brainstem stroke may cause lower motor neuron involvement.) Paralysis of the forehead muscles suggests lower motor neuron weakness and Bell palsy, whereas preservation of the forehead muscles reflects an upper motor neuron lesion and a stroke. In addition, most strokes that cause facial weakness have other symptoms and signs, such as arm numbness or weakness on the same side.
Hypoglycemia
Defined as a patient with a dangerously low blood glucose level, hypoglycemia can cause symptoms similar to those associated with a stroke. However, a doctor should be able to determine whether hypoglycemia is causing the symptoms fairly quickly by testing the patient’s glucose level.
Tumor
Whether cancerous or not, a brain tumor can cause symptoms that mimic a stroke. The primary difference is that tumor symptoms tend to increase gradually in severity as the tumor grows whereas stroke symptoms tend to present suddenly and acutely. But this distinction can be of little use to a doctor when a patient arrives to the hospital having lost consciousness.
Seizures
Seizures and post-seizure events can cause alterations in brain functioning that mimic the symptoms of a stroke. If the doctor observes the seizure or is told of a history of seizures, the doctor may be more likely to diagnose a stroke as a seizure-related impairment of brain functionality.
Factors That Contribute to Misdiagnosis of Stroke
A recent study from Johns Hopkins University concluded that doctors overlook or discount the early signs of potentially disabling strokes in tens of thousands of Americans each year. The study, which analyzed data from nine states, found that:
- Patients whose stroke was misdiagnosed disproportionately complained of dizziness or headaches and were told they had a benign condition, such as inner-ear infection or migraine, or were given no diagnosis at all.
- Up to 12.7 percent of people turned away and later admitted to the hospital for stroke had been potentially misdiagnosed and erroneously sent home from an ER in the 30 days prior to their eventual hospitalization.
- About half of stroke patients who returned were back in the ER within seven days, and more than half of those patients returned within the first 48 hours.
- Women were 33 percent more likely to be misdiagnosed.
- Minorities were 20 to 30 percent more likely to be misdiagnosed.
Nationwide, the estimated number of misdiagnosed strokes resulting in harm to patients, based on the data in the study, could be between 15,000 and 165,000 annually.
Strokes are often misdiagnosed because there are several conditions that mimic the symptoms of a stroke, and because a stroke is incorrectly seen as something suffered only by elderly patients.
The failure to correctly diagnose can occur if health providers:
- Fail to take a thorough medical history or to perform a proper physical examination
- Fail to order the right diagnostic studies that can identify a blockage or rupture
- Misinterpret test results
- Fail to recognize stroke symptoms in patients who otherwise appear healthy
- Fail to distinguish stroke from similar conditions
Management of Stroke
In any patient presenting to the ED with signs of an acute stroke, the goal of management is to determine whether or not the patient may benefit from revascularization. The patient must be stabilized, undergo CT imaging of the brain that is performed and interpreted by a radiologist, be clinically evaluated with a pertinent history and physical examination, and have laboratory studies completed within 60 minutes of arrival.
Quantification of Neurologic Impairment
The NIH developed a 42-point stroke scale (NIHSS) that allows quantification of neurologic impairment. This scale provides insight into the location of vascular lesions, is correlated with outcomes for ischemic strokes, and identifies patients who are candidates for thrombolytic therapy. Points are assigned on the basis of performance in six major areas: level of consciousness, visual function, motor function, sensation, cerebellar function, and language. The scale is used at the initial presentation and can be repeatedly employed over the hospital course to assess the evolution of the patient’s neurologic status. Patients with minor strokes usually have a score of less than 5.
Stroke Evaluation Time Benchmarks for ED-Based Care
Time interval Time Target
Door to doctor ≤ 10 min
Access to neurologic expertise ≤ 15 min
Door to CT initiation ≤ 25 min
Door to CT interpretation ≤ 45 min
Door to treatment ≤ 60 min
Admission to stroke unit/ICU ≤ 3 hour
Thrombolysis
Guidelines from the American Heart Association/American Stroke Association on the early management of acute ischemic stroke recommend the off-label use of tissue plasminogen activator (t-PA) within 3-4.5 hours after symptom onset, based on findings from the third European Cooperative Acute Stroke Study trial. Another recommendation is that door-to-needle time be within 60 minutes for patients eligible for thrombolysis.
Considered the gold standard, tissue plasminogen activator (or Alteplase IV r-tPA) is the only FDA-approved treatment for ischemic strokes.
- When promptly administered, it can save lives and reduce the long-term effects of stroke.
- Alteplase IV r-tPA is given through an IV in the arm, and works by dissolving the clot and improving blood flow to the part of the brain being deprived of blood flow.
- Alteplase IV r-tPA needs to be used within three hours of having a stroke or up to 4.5 hours in certain eligible patients.
- Many people miss this key brain-saving treatment because they don’t arrive at the hospital in time for Alteplase treatment, which is why it’s so important to identify a stroke and seek treatment immediately for the best possible chance at a full recovery.
Thrombolysis in Children
In most adults, stroke is due to atherothrombotic disease. In kids with strokes, it is due to a number of different etiologies, including sickle cell disease, moyamoya disease, genetic disorders, structural disorders of the brain and blood vessels, and the like.
In a study that looked at treatment of children with ischemic stroke, out of their cohort of several hundred patients with stroke, only 2% of them ended up getting IV tPA. Overall, the kids who got IV tPA had a worse outcome than children with strokes who, for various reasons, did not get IV tPA.
Other recent studies have also shown that pediatric patients with ischemic strokes may not benefit from IV tPA therapy. At this point, the recommendation is to avoid IV tPA therapy, and in some cases clot removal, in a pediatric population with ischemic stroke. In these patients, many of whom are too young to consent for themselves, there needs to be a full and engaged discussion between the healthcare provider, the patients’ parents, and the patients themselves so that we fully understand the risks and the benefits of tPA and/or endovascular therapy in this group.
Endovascular Therapy (EVT)/Mechanical Thrombectomy
Although intravenous t-PA is the primary medical therapy for acute ischemic stroke, American Heart Association/American Stroke Association guidelines also recommend physical removal for large-vessel occlusion to restore blood flow during an acute ischemic stroke in patients who are ineligible for or fail intravenous t-PA.
The gold standard for mechanical thrombectomy in ischemic stroke is the stent retriever, which has shown improvements in clinical outcomes versus t-PA alone in at least five clinical trials. This treatment should be implemented within 6 hours of acute stroke symptoms and only after a patient receives t-PA.
Aspiration may be tried if a stent retriever is not successful. In aspiration, a large-bore aspiration catheter is used to remove the blood clot via negative-pressure. Aspiration may be quicker than stent retriever from clot contact to restoring flow (13 minutes vs 23 minutes). This could be important, as time is brain.
The potential complications of aspiration catheters are distal embolization of fragments and occlusion of collateral pathways through the anterior communicating artery with large-bore catheters.
The race of the patient can also play a role in choosing which method to use. African Americans, Hispanics, and Asians generally have more intracranial atherosclerosis — hardening of the arteries, which may cause stenosis — and in these cases, aspiration may not be enough. It may pull the clot out but the stent in the stent retriever also opens up the artery. So, in these patients a stent retriever may be better.
In the 80% or so of patients eligible for intravenous t-PA, this procedure is ideally administered under the guidance of a stroke physician with specialized training in stroke care. About 20% of patients with ischemic stroke might be eligible for EVT. If, on the basis of examination and results of neurovascular imaging, the stroke physician recommends EVT, he or she will contact an endovascular colleague.
For patients with hemorrhagic primary or conversion strokes or those with life-threatening elevation of their intracranial pressure, urgent neurosurgical consultation is required. If there is concern about possible herniation, surgical decompression may be necessary to evacuate a hematoma. Hemorrhagic conversion of an ischemic stroke renders the patient ineligible for t-PA and at greater risk for elevated intracranial pressure.
Mechanical Treatment for Aneurysms and Arteriovenous Malformations or AVMs
- A small tube called a catheter can sometimes be threaded up through a major artery in an arm or leg and guided into the brain tissue, allowing the surgeon to use camera technology to help fix the problem.
- Once the catheter is guided to the source of the bleeding, it deposits a mechanical agent, such as a coil, to prevent further rupture.
- Sometimes surgery is required to secure a blood vessel at the base of the aneurysm.
Treatment to Lower Risks of Stroke
The good news is that 80% of strokes in adults are preventable; however, after having a stroke, risks are much higher for having another one. Preventing a second stroke can be the most important treatment of all.
Adopting healthy lifestyle habits and managing key risk factors, including high blood pressure, cigarette smoking and atrial fibrillation can make all the difference.
More than half of all strokes are caused by uncontrolled hypertension or high blood pressure, making it the most significant risk factor to control.
Medical treatments may include:
- Medications to control high blood pressure.
- Medications to manage atrial fibrillation among high-risk patients.
- Medications to lower the chances of forming a clot (Antiplatelet agents or anticoagulants, such as warfarin, interfere with the blood’s ability to clot and can play an important role in preventing stroke).
- Procedures to remove plaque buildup or open blockages.
Telemedicine
Telemedicine stroke centers are an area of active research and funding by federal and state governments. Specialty maps can identify which patients are within driving distance of major stroke centers and which patients can be connected via remote video conferencing. Experts in stroke care can remotely assess a patient’s stroke risk and determine whether immediate transfer to a major hospital is warranted. The goal is to get at-risk patients to hospitals where they can be treated with fibrinolytics within 4.5 hours of symptom onset.
Treatment of stroke is a continuum that begins with prehospital care and ends with discharge. Patients with ischemic stroke may benefit from one of several therapies, depending on the location of the lesion, the time since onset, and concomitant medical conditions. For patients who present with an anterior circulation stroke within 3-4.5 hours of onset and without a contraindication, thrombolysis with intravenous t-PA is a proven measure. Compared with patients given placebo, patients given t-PA have less disability as measured by the Rankin Scale of Global Disability, where 1 represents no significant disability and 6 represents death. For patients who present within 6 hours of symptom onset, there is a growing body of evidence suggesting that intra-arterial t-PA may be effective. Promising news came from a number of clinical trials that showed that intra-arterial intervention within 6 hours of stroke onset, coupled with intravenous t-PA, significantly improved outcomes in patients with acute ischemic stroke caused by a proximal intracranial occlusion of the anterior circulation.
Monetary Damages
These can include current medical bills and projected medical and rehabilitation expenses, as well as lost wages and future earning potential.
Non-economic Damages
These can include physical or mental pain and suffering, and loss of companionship. In the case of death as a result of medical negligence, the patient’s family can receive monetary compensation on the “full value” of a life
Liability for Misdiagnosing a Stroke
Because symptoms of a stroke can resemble some other medical problem, misdiagnoses are not uncommon – but that doesn’t get the doctor off the legal hook.
When a patient suffers a stroke, the first few hours afterward are critical. If an emergency room doctor or staff member does not diagnose and treat the condition quickly, or if they misdiagnose it, the patient may suffer reduced mental capacity, permanent brain damage, and even death. Speed of treatment is the primary determinant of how severe a stroke’s effects may be.
Call us today or fill out our online contact form for an evaluation of your case.


Leave a Reply
Want to join the discussion?Feel free to contribute!