Acute Complications of Spinal Cord Injury (SCI)
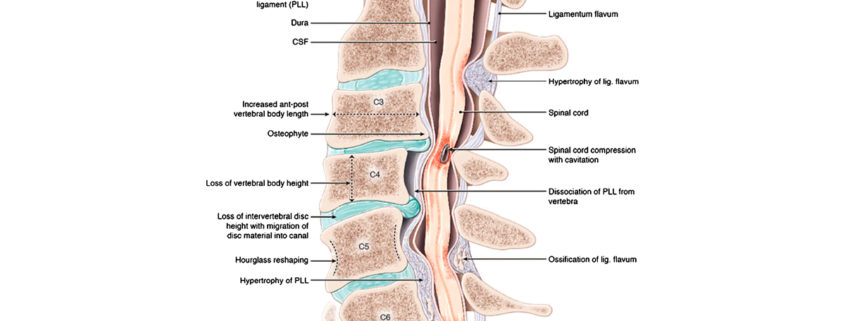
The spinal cord is a delicate, glistening, rope-like bundle of nerves that connects the brain to the rest of the nervous system. It is bathed in cerebrospinal fluid and held in place by ligaments and nerve roots inside the spinal column. While the spinal cord itself is elastic, stretching with every turn of the head and bend of the waist, it is exquisitely sensitive to pressure. Few spinal injuries sever the cord completely, but fatal or paralyzing injuries can result even when the cord is bruised, twisted, pinched, or stretched. The higher up in the neck an injury occurs, the more potentially life-threatening it is because it may cut off the brain’s communication with all the nerves below it.
The cervical spine has seven vertebrae, C1 through C7. Each vertebra guards a different set of nerve roots. Any break in the first four vertebrae resulting in serious injury to the spinal cord can cause severe impairment of breathing and quadriplegia. The nerves that control breathing are mainly in the C3 and C4 area. All the nerves that control the movement of the torso, arms, and legs are below.
Cervical injuries can have serious effects on the respiratory system, and respiratory failure is one of the major complications and a frequent cause of death both in the acute and chronic phases. In the acute phase, 84% of patients with injuries above C4 and 60% of patients with injuries between C5 and C7 will experience respiratory difficulties within days of an injury, and 75% to 80% of patients with quadriplegia above C4 and 60% of those with quadriplegia caudal to C4 will require invasive mechanical ventilation. Additionally, a total of 65% of patients with injuries between T1 and T12 will experience severe respiratory complications.
Inspiratory capacity is usually diminished in patients with higher level spinal cord injuries, contributing to micro atelectasis (36.4%), dyspnea on exertion, and, in patients with more severe impairments, respiratory failure (22.6%). A 30% to 50% reduction of vital capacity may occur during the first week in patients with injuries at C5-C6. Close surveillance of respiration is important. Vital capacity and arterial blood gases should be measured until the patient is stable.
The muscles of expiration are impaired in many people with spinal cord injuries above T8, resulting in profound effects on coughing, clearance of secretions, and susceptibility to lower respiratory tract infections such as pneumonia. In those with higher lesions, asthma-like disorders of airway function may occur, which can be prevented by cholinergic antagonists. This abnormality has been attributed to the unopposed effects of parasympathetic innervation on respiratory smooth muscle resulting from the disruption of sympathetic efferent neurons.
Contusion injuries in which the spinal cord is incised on either side at the second cervical segment (C2) effectively interrupt the descending respiratory projections to the phrenic nucleus ipsilateral to the hemisection, thereby paralyzing the ipsilateral hemidiaphragm and resulting in a significant reduction in tidal volume and an increase in breathing frequency. The phrenic motor neurons in the ventral horn of the cervical spinal cord extend rostrocaudally as an interrupted column of cells. The specific segmental location of phrenic neurons is between C3 and C5.
In clinical studies, spinal cord injuries with MRI evidence of cord contusion or hematoma had poor neurologic prognoses—the prognosis was better when edema only of the cord was present.
Spinal Cord Injury (SCI) causes alterations in neurotransmitters and proteins both below and above the injury, resulting in further SCI called “secondary SCI.” The cause of injury is not fully understood, but it seems multifactorial, including blood flow changes, edema, hemorrhage, electrolyte abnormalities, membrane injury, and release of cytotoxic mediators and excitotoxic neurotransmitters.
Excitotoxic neurotransmitter release can increase intracellular calcium and cause further spinal cord damage. The result of these processes is lethal injury to a cell that had initially sustained a reversible injury, thereby limiting recovery from a spinal cord injury.
After a high cervical SCI, changes in protein levels extend into the brainstem. Changes in protein levels within the brainstem could potentially cause a direct change in the respiratory motor output, as well as alter other autonomic control systems located within brainstem regions.
Inflammation
Inflammation is an expected response to injury, but in spinal cord injuries, inflammation can produce devastating results. With little or no room to expand as the cord swells, its blood supply is impaired, which causes further damage to the delicate tissues.
Prior to the past few years, there was no immediate treatment for spinal injuries beyond the basics of trauma care: immobilizing the neck to prevent further injury, restoring pulse and breathing, and replenishing fluids. Several studies since then have shown that patients with spinal cord injury, complete or incomplete, presenting within hours of the acute event have done better when they were promptly given an anti-inflammatory steroid called methylprednisolone. Methylprednisolone is thought to reduce nerve damage by slowing inflammation and other harmful biochemical reactions that are part of what doctors call the “secondary trauma” of a spinal cord injury, i.e., trauma that occurs beyond the initial event.
Methylprednisolone is given within eight hours of an injury and in massive doses—about 1,000 times the normal amount of steroids the body uses in a day. The usual regimen is methylprednisolone 30 mg/kg bolus over the first hour, followed by a continuous infusion of 5.4 mg/kg/h for 23 hours.
Other Complications of SCI
In addition to motor and sensory deficits, instabilities of the cardiovascular, thermoregulatory, and other systems are common after an SCI. Disturbances of the urinary and gastrointestinal systems are typical, as well as sexual dysfunction. Frequently seen complications of cervical and high thoracic SCIs are neurogenic shock, bradyarrhythmias, hypotension, ectopic beats, abnormal temperature control, and disturbance of sweating, vasodilatation, and autonomic dysreflexia.
Autonomic dysreflexia is an abrupt, uncontrolled sympathetic response elicited by stimuli below the level of injury. The symptoms may be mild (like skin rash or slight headache), but the response can cause severe hypertension, cerebral hemorrhage, and death. All personnel caring for the patient should be able to recognize the symptoms and be able to intervene promptly.
Additionally, due to physical inactivity and altered hemostasis, patients with SCIs have a higher risk of venous thromboembolism and pressure ulcers. Spasticity and pain are frequent complications that need to be addressed. The psychological stress associated with SCI may lead to anxiety and depression. Knowledge of possible complications during the acute phase is important because they may be life-threatening and/or lead to prolonged rehabilitation.
Treatment
The role of surgical intervention for acute spinal trauma—namely, neural decompression, spinal reduction, and stabilization—is somewhat controversial. The aim should be early surgical fixation wherever possible, even in elderly patients, if there is no significant comorbidity or contraindication for surgery.
It is important to distinguish between compressive versus non-compressive myelopathy. This distinction helps to identify conditions amenable to early surgical management.
Decompressive surgery in a patient who is neurologically intact, followed by fixation/fusion, should be performed under optimal conditions to preserve cord function. A more controversial situation occurs in a patient with a partial spinal cord injury and ongoing compression who is deteriorating clinically. Based upon the pathophysiology of secondary injury, the presence of cord compression may impede regional blood flow at the site of injury and promote secondary injury. Therefore, removal of the compressive condition—a disc herniation, a bone pressing on the spinal cord, a blood clot—may optimize the regional milieu within which the spinal cord can recover and potentially counteract some of the factors involved in accelerating secondary spinal cord injury.
Surgery cannot repair a severed nerve or heavily damaged spinal cord and restore, for example, the ability to breath. In fact, surgery would be contraindicated if the patient’s cardiorespiratory status were unstable, as operating under such conditions could exacerbate secondary spinal cord injury.
Contraindications to surgery include debilitating cardiac or pulmonary disease, short life expectancy (especially less than six months), and multilevel vertebral disease that prohibits reconstruction and stabilization.
It may be necessary to stabilize the head and spine of a patient with a broken neck; however, reduction and stabilization remain strictly elective procedures. Until surgery is carried out, there are effective means of immobilizing a patient without surgery to prevent further spinal cord injury.
Prognosis
Despite significant advances in treatment protocols and operative techniques, the ultimate prognosis for acute traumatic spinal injuries is determined by the extent of the initial injury and the level of the spinal column affected—the lower the injury in the spinal column, the more favorable the prognosis. People with quadriplegia due to an injury to the lower neck (for example, the sixth cervical vertebra) may recover well enough to feed themselves, walk in leg braces, and drive a vehicle. Some quadriplegic patients can have children.
During the first year after injury, improvements in respiratory function occur spontaneously, and only 5% of patients require ventilatory support. Even in patients with lower level quadriplegia and paraplegia, improvements in lung function are observed over the first year. This is not unusual because small improvements in general motor function usually occur during the first year after injury. After the first year, very little improvement is noted—indeed, sometimes loss of function is observed. Gains in function of respiratory musculature after SCI, whether occurring spontaneously or stimulated by rehabilitation paradigms, point to the plasticity of the nervous system and its ability to form new connections after SCI.
A complete spinal cord injury, defined as no spinal cord function below the level of the lesion, is almost certainly not expected to regain neurologic function despite intervention.



Leave a Reply
Want to join the discussion?Feel free to contribute!